We understand the frustration and concern many patients seeking breast reconstruction are feeling during this time. Because of the COVID-19 outbreak, most reconstructive surgeries are being delayed for the safety of patients and to help conserve much needed PPE for healthcare workers on the front lines of fighting this virus. To help erase any confusion and provide as much information as we can, Dr. Chrysopoulo hosted a Facebook Live question and answer event where he answered your top questions regarding COVID-19 and breast reconstruction. If you missed it, no worries! You can catch the replay below. Don’t have time to watch the whole thing? Scroll below for an overview of each question asked and Dr. C’s response. We hope you find this helpful!
Question: What is COVID-19?
Answer: COVID-19 isn’t the virus. COVID-19 is the disease the corona virus causes. Corona virus is the name given to the SARS CoV2 virus (that’s the formal medical name. It’s important to note here that it’s got nothing to do with the flu. It’s been compared to the flu, but it’s not the flu. It’s not an influenza virus (that is the same type of virus family that causes the flu). But some of the symptoms initially can be similar. The symptoms of a COVID-19 infection can be fever, a dry cough, shortness of breath especially on exertion (if you’re doing something and all of a sudden you’re a bit short of breath and you kind of think that’s weird then that may be the first symptom that you have), fatigue, poor appetite headache, and some people also have GI symptoms like diarrhea. Please don’t go and hoard toilet paper…there’s really no need! It’s important to bear in mind too that at least 25% of people who become infected with the
corona virus never develops symptoms. That’s why a social distancing is really important! Stay six feet from anyone when you leave the house. Obviously inside the house with your loved ones it’s very difficult to stay six feet away and there’s really no need to social distance from them. Unless there’s a concern a family member has been exposed. In that case, please try at all costs if it’s possible to separate that individual from the rest of the family.
A lot has been made of the fever because it’s such a common symptom. You don’t need to have a fever to develop COVID-19 or to have COVID-19. In fact, all of those symptoms I mentioned above can occur on their own. For example, I have a very close friend who was recently admitted to hospital for care and he just felt fatigued for many days before the shortness of breath kicked in. He never actually had a fever at all and we are hearing more and more of those cases.
Question: How is COVID-19 spread?
Answer: First and foremost, this is a respiratory disease. The virus attacks your lungs first before it attacks anything else. that’s how it really tries to get a hold of your body is through your lungs. Coughing, sneezing and even breathing can spread the virus. Anything that releases droplets into the air can spread the virus. That’s why the social distancing is really being emphasized because the best way to protect yourself is to stay away from other–at least six feet. You can also develop the inflection through touching someone who’s infected or come into very close contact. Doesn’t have to be a droplet! The virus can get on your hand and then you touch your face. If you touch your mouth, your nose or your eyes that’s how the virus then gets into your system, because it was on your hand.
Coronavirus can stay alive outside the body for many hours, and depending on the surface, for many days. Metal surfaces in particular can have corona virus on them. (Examples: doorknobs and shopping carts) The virus can stay on metal 3-5 days according to some studies. When you look at the cruise ship data, there’s some evidence that the virus can live up to nine days. If that’s true it probably has to do with environmental conditions like sunlight and heat. We just don’t know quite frankly, but what we do know is the virus survives on metal for at least three days. So if you have to go to the grocery store wipe down the cart. I would also recommend that you wear gloves. There’s been a shift in terms of the recommendations for face masks. Initially the CDC and the World Health Organization stance was that you didn’t need to wear a face mask unless you were sick. The reason for that being that face masks really weren’t that protective if you weren’t sick already and the reason to wear a mask if you were sick was basically to keep the virus to yourself and to prevent spreading it. But I’m sure those of you who have been watching the news and the images from around the world from the countries that have dealt with the virus more successfully than the US (places like South Korea, Hong Kong, Singapore)the public is walking around with a mask. Now the sense is that there’s something to that and even though face masks won’t protect you 100% the recommendation now has shifted. I would say if you’re going out to a store or grocery store wear a mask of some sort. If you don’t have a mask wear a bandanna over your nose and your mouth. It’s better than nothing. I do feel very strongly that we have to prioritize the safety of our first-line health care workers. A lot of them are dealing with patient after patient after patient who are infected. Our first-line health care workers must be prioritized in terms of face masks and other personal protective equipment. But, in terms of what our patients should do…if you have a mask at home—great! Please don’t hoard stuff if you don’t have a mask. it’s okay just wear something like a bandanna. Even that will help.
Question: What can individuals do to protect themselves?
Answer: In addition to what we’ve just said think about what you’re touching. Hopefully you’re all social distancing you will staying at home. If you’re not, you should be. It’s the only way to stop the transmission. If you think about people as dominoes, when you line up dominoes and then you flick one, each domino eventually falls after you flip the first one over. If you imagine each domino to be a person and the virus spreads from person to person, just by being close to each other. that first person who gets infected potentially infects three other people. The only way to stop the dominoes from falling is to move a couple of dominoes out of the way so that when the last domino falls it doesn’t touch the next one and doesn’t push the next one over. That’s how social distancing works. The infection stays in those infected folks, doesn’t spread, and eventually it dies out and that individual hopefully gets better. Most people do get better! For the 20% of people who get symptoms, the symptoms are mild. Another 20% of folks will have more severe symptoms but probably won’t need to be hospitalized. It’s only about 10-15% of people who get the infection that will need hospital care and of those it’s about 5% that will have severe breathing problems that will potentially need intensive care unit ventilators.
Question: Who is at risk for developing severe symptoms?
Answer: The elderly and people with underlying medical problems are most at risk. This includes those who have compromised immune systems. So obviously cancer patients are very much on that high-risk list. Now, if you’re a ten-year survivor or you’re ten years out from chemo, you’re not considered immunocompromised anymore and you’re not high risk. But, if you’ve just finished chemotherapy you’re high risk. If you’re going through cancer treatment right now, if you have a current cancer diagnosis–you’re high risk. So, you must protect yourself and really minimize your contact with the outside world. Minimize doctor visits as much as you can. Obviously, that’s impossible if you’ve got cancer treatment still going on and you need to go in to see your oncologist. But you finish treatment or you’re not getting active treatment right now don’t go for a mammogram or for your ultrasounds. All those things can wait. The American Society of Breast Surgeons has recommended very strongly that all screening tests to be postponed.
Question: Why have hospitals canceled breast reconstruction surgeries?
Answer: There are a bunch of recommendations now from American societies (the American College of Surgeons, the American Society of Breast Surgeons and the American Society of Plastic Surgeons. Any breast cancer care that doesn’t involve surgery is essentially being prioritized. If there’s any possible way you as a breast cancer patient can be treated right now without surgery initially without it impacting your prognosis then that’s the recommendation. For example, if your cancer can be controlled by hormone therapy, an aromatase inhibitor or you can have neoadjuvant chemotherapy first before your surgery, all that’s going to be prioritized. We want to keep people out of hospital as much as possible. The last thing breast cancer patients who are immunocompromised need is to go into surgery and be exposed to the virus. As I said, this affects your breathing, your lungs, your pulmonary, and your respiratory system. The last thing you want to do is go into surgery for a surgery that could have potentially been delayed a little bit and then you end up on a ventilator because you contracted the virus. This is also about preserving resources to get all the COVID-19 infected patients through this and minimize the death rate. But please know, this decision from our society’s in terms of breast cancer care is to protect you. Please remember that a breast reconstruction as a result (because the surgery is not immediately life-saving) is going to be postponed. Certainly here in Texas that’s the position. In certain situations in parts of the country (depending on the geographic situation and how bad things have gotten) it also depends on your state laws. There have been several state laws that have been passed that prevent certain surgeries. Please talk to your medical team your and your surgical team about your specific situation. But basically, breast reconstruction is on hold because it’s been deemed that it’s not immediately life-saving. Unfortunately that really does prolong the process for many people. Lots of patients have now been caught in limbo but you will get through this. You will get your surgery. I don’t know when things are going to be back in terms of scheduling. Certainly for us for us, we’re looking at this in two week increments moving forward and it’s a very fluid situation. Numbers are changing, the infection numbers are changing, the projections are changing. It’s a day-by-day thing. We just have to prioritize everyone’s safety.
Question: When will people being rescheduled for surgery?
Answer: All I can say is they’ll be rescheduled as soon as it’s safe to do so.
Question: Can you get the virus again if you’ve already been diagnosed?
Answer: We think that if you get it once that you’ll be okay for this season. I mentioned at the beginning that coronavirus is an influenza-like virus BUT it’s not the flu. But in terms of immunity, it probably is quite similar. When you get the flu it doesn’t mean you can never get the flu again, but it does mean that if you do get the flu again it won’t be quite as severe. Your immune system does protect you somewhat for the following season. Obviously the flu shot is a big help! I’m not going to get into the whole pros and cons of vaccination. Personally everyone in my family will always be vaccinated because vaccines work. But let’s not talk about the pros and cons of vaccines in this Facebook Live. Hopefully the vaccine for coronavirus or for COVID-19 will be available soon. When you look at how long it takes to develop a vaccine (and several companies are working on it already) realistically it’s not going to appear I don’t think before the beginning of next year at the very earliest. It looks like right now that if you get COVID-19 you should be okay and you won’t get it again. But we don’t know for sure how long can someone be a carrier. I don’t know the answer to that because without widespread testing we don’t know who is a carrier so we don’t know how long they’ve been carrying it. If you look at the lifespan of the disease if you get through two weeks (which is why for folks who are in quarantine it’s two weeks to make sure that it that they don’t develop any symptoms) we think the virus kind of burns itself out…but we don’t know for sure. There have been a small percentage of people who have become infected and ultimately didn’t develop symptoms until beyond two weeks but that’s only about 1% of people who have been infected as far as we know.
Question: Is there any medicine that we can take to help?
Answer: To help stop the intensity if you start feeling symptoms but don’t know if it’s in fact COVID-19, no treatments that we know of that have been proven to be effective. Obviously there’s a lot of hope being put on hydroxychloroquine and z-pack but the data on that is very poor to be honest. In terms of vigorous scientific data, if you develop symptoms the only thing you can do really it’s make sure you stay well hydrated, and make sure you’re still eating as much as you can. It’s supportive measures only really.
Question: Is there a blood test for antibodies to determine if you’ve already had COVID-19?
Answer: It’s coming. It’s not it’s not here yet and it’s not going to be widely available for awhile, but it’s coming.
Question: If someone completed radiation treatments eight years ago and they are 65 and they have a compromised immune system should they be going to work?
Answer: I wrote an article on that published on BreastAdvocate.com. It’s about what coronavirus is and what breast cancer patients should know. There’s a whole list of precautions, advice and one of those is if there’s any way you can work from home do it. Again going back to social distancing…you know we’re at the point where this isn’t going to go away on its own. There cannot be life as usual. The best thing anyone can do to protect themselves is limit their risk of exposure. The only way to do that is to stay home and leave the house only when you absolutely must. When you go out be a minimum of six feet away from everyone. That means most people should be staying at home and working from home if that’s at all possible. Now I fully appreciate that unless it’s mandated by your individual state it’s very much left up to your employer, but please push it as much as you can to work from home.
Question: I was supposed to have prophylactic surgery this year but it’s been postponed. Should I ask my doctor about going on tamoxifen?
Answer: That’s a great question. Anyone who has a high-risk gene mutation, anyone who carries a gene mutation like BRCA (which is obviously the best known but certainly not the only one) should talk to their physician about steps that they can take that don’t involve surgery to see them through until the point where they can get surgery. Please also remember that non-surgical methods of risk reduction are chosen by a lot of people right off the bat. It’s a very valid way to go to decrease your risk. As I mentioned earlier the screening aspect of it is going take a hit for the next few months, but you can definitely go on risk reducing medications like tamoxifen.
Question: If it does not impact prognosis and local hospital resources allow for a choice between hormone therapy or a mastectomy is it still preferable to opt for immediate mastectomy with DIEP flap later?
Answer: Well if it doesn’t impact your prognosis then you can also look at it the other way and ask, ‘why have the mastectomy if that can be delayed.’ From a from a strictly cosmetic standpoint, immediate reconstruction is going to be better. In some places you can still have your mastectomy and have a tissue expander placed. The tissue expander preserves the skin envelope and you can later have that expander exchange for your DIEP flap, so in that sense you do get an extra surgery because the DIEP flap and the mastectomy aren’t being performed at the same time but the tissue expander is used as a bridge between the two. Whether that’s an acceptable way to go or not will depend on where you are and the situation. Primarily state laws right now
Question: Does PRMA perform reconstruction surgery for patients outside of the US?
Answer: Absolutely! Not right now though. Right now at PRMA we’re really not doing any breast reconstruction unfortunately but that’s beyond our control. That’s what has to happen right now. The only procedures we’re performing are for patients who have recurrent cancer who need what we call “soft tissue coverage,” but that’s a life-saving procedure. It goes beyond a breast reconstruction…it’s more of a wound closure. We’re not performing any breast reconstructions right now at PRMA. We hope to get back as soon as possible and we certainly will as soon as it’s safe. We operate and we see people from all over the country and abroad. So far as our international folks, obviously there’s the added dimension of air travel and when it’s safe to do so. We will always prioritize patient safety, but we very much welcome patients from all over the world. For anyone who’s considering coming, now is a great time to have a telehealth visit with any of our physicians just so you can get your options.
Question: Once we get back to normal and you are allowed again to do surgery, how long would it take to be scheduled again?
Answer: Great question! But I don’t really know. Right now there are seven of us in terms of surgeons at PRMA. I’m going answer this specifically in terms of PRMA because I can’t speak to anywhere else in the country or any other countries for that matter. For us in San Antonio, PRMA specifically, we have seven surgeons. We are all in touch on a daily basis and we all feel the same way. We’re all very passionate about this. We’re on sabbatical right now. Essentially, I told my wife that this is the vacation for the year so we’re all going to be working very hard once the operating rooms are opened up. I promise and we will get everyone in as soon as we can. Unfortunately, some of you will have to wait a little bit longer then you want to wait, but we’re going to get everyone through as soon as physically possible. I promise!
Question: How would we go about getting a conference with you?
Answer: Go to our virtual consult page on our website PRMA-enhance.com and click on the Virtual Consultation button. It’s that simple. We look forward to hearing from you.
Question: What is your advice for staying healthy while patients are waiting for the DIEP flap procedure and sheltering in place?
Answer: Great question! Nutrition, nutrition, nutrition! And exercise. Don’t start any bad habits. Don’t start smoking. You can still drink, just use your best judgment and also obviously follow your medical oncologist guidelines in terms of alcohol because you may be on some other medications…it depends on what part of your treatment you’re in etc. But nutrition is really important. Just try to eat as healthy as possible and exercise. Aerobic exercise always improves healing so try and get some exercise in if you’re waiting for a DIEP flap. Specifically remember what your surgeons told you in terms of where you are with your specific weight. Sometimes losing a significant amount of weight can hurt you in terms of the DIEP flap procedure and how much tissue can be moved and how much tissue there is to work with or any other flap procedure for that matter. So I wouldn’t prioritize weight loss but I would prioritize healthy living as much as possible.
Question: What should individuals do about abdominal wounds that aren’t healing properly during this time?
Answer: It depends on the practice that you’re in and who your physician is and how they do it, but I’ll tell you how we’re doing it a PRMA. If one of my patients has a wound healing problem, the first thing we’re going to do is get on telehealth and take a look at things and see how things look. Not all healing problems are the same so if we see that it’s just a little bit of superficial scabbing or something then a little TLC is all the patient needs then that person isn’t going to have to come in and increase their risk of exposure by coming into a medical office. If it’s something that looks like needs to be cleaned up and we need to maybe breed or cut away a little bit of tissue to help things heal then we’ll have you come in. It evaluated on a patient by patient basis. Let me also backtrack a little bit and tell you what we’re doing in the office again in case you do still have to come in for an in-person visit. Let’s say you do have a wound healing problem or let’s say we’re worried about an infection or a hematoma bleeding or anything that cannot be dealt with over telehealth. We, for many weeks now, have been following the most aggressive approaches in terms of minimizing risk in the office so please be prepared. The nurse and the physician wear masks gloves. It’s not personal it’s for everyone’s protection. Everything is cleaned with antiviral detergents between every visit. People will be staggered so the only person who will be in the office when you’re there will be you unless it’s impossible to avoid that situation. That’s always going to be the primary goal. If there’s someone else already in the office and you have to wait a little bit for the appointment then you’ll be asked to wait in your car outside and we will text you or call you (whatever works best for you) when we are ready for you to come in. We’ve got this really streamlined now. We take this exceptionally seriously and we’re only going to be bringing you into the office if we absolutely have to.
Question: I am a five-year survivor with asthma and on tamoxifen. Am I considered high-risk?
Answer: Yes, anyone with a breathing issue like asthma, chronic bronchitis, COPD, smokers, anyone who vapes are high-risk. You don’t have to smoke cigarettes; it includes pot as well. Anything you inhale increases your risk because it really decreases your capacity to deal with a pulmonary insult. Anything that attacks your lungs is going to have an easier time if your lungs are compromised because you inhale stuff on a regular basis, that is more than just air. We have seen a lot of younger folks be hospitalized and we think that some of that is the extent of vaping in that age group.
Question: I am two-weeks post-op double mastectomy with DIEP flap. Because of COVID-19, will my phase 2 surgery be delayed?
Answer: Yes, all surgeries are off right now. So yes, unfortunately your revision will be delayed. For surgery in our practice, most people get a stage two, or a tune-up surgery, revision surgery. Step one, the first surgery, is about making patients physically whole again. Then the second surgery is about making them look as good as possible. This addresses symmetry issues, size discrepancy, contour issues after mastectomy, and maybe some unevenness and scarring. If you have had DIEP flap surgery, we address the belly scar to smooth things out and smooth out the belly contour; basically, make things look as good as possible, that is stage two. So yes, all stage two surgeries are also delayed.
Question: Since I was scheduled for this week, I have been following pre-op instructions, should I continue?
Answer: That’s a good question, some of them you’ll need to continue, others not so much. So I would say if you are a PRMA patient, please email your nurse and get in touch and go through the list to see which of those you really need to be continuing, and which of these you can put on hold for now. Great question.
Question: I am assuming that the length of time for a tissue expander placement is not a problem? I have some family members that are concerned I have had a tissue expander in place for 2 years, and now it is up in the air – is there a limit on how long the tissue expander can be in place?
Answer: No, if you are not having any problems and you’ve got a tissue expander in place, and you are not having any issues, you can keep that in for as long as you need to. So no, it is not a medical concern, it doesn’t impact your health if you’ve got no problems with it whatsoever. Rest assured there is no urgency from a medical standpoint or health perspective. I know you’re probably dying to get it out, but medically speaking you’re fine.
Question: Can you demonstrate proper hand washing?
Answer: I can try. Okay, take off your jewelry. Warm water and soap will do it. So nothing special, right? Quite frankly if you’re in the kitchen and you’ve got dish detergent, that will work. Warm water, and you’ve got to wash your hands for at least 20 seconds. There have been some pretty amusing songs on social media of people picking different songs. Do whatever you need to do that lasts 20 seconds to guide you. You get your hands wet with warm water, add the soap or detergent, lather up, get a nice foam. I would treat this kind of like a pseudo surgery scrub. You know when we prepare for surgery, where obviously we do a lot more than this, but this is kind of a pseudo hand washing. So once you’ve done that for a few seconds, focus on every finger, and both thumbs, all the way around each finger, all the way around both thumbs. Then you do one hand on top of the other, because you need to do that to really get into the webbed spaces. Every webbed space, and then again on the other side once again to finish off. Then get your jewelry, rinse that and wash it really well. This ring is metal, and the virus can live on metal of days on end. So wash It really well, then put it back on and dry your hands. That’s it! 20 seconds, warm water, with soap!
Question: What is the optimal BMI for DIEP flap surgery?
Answer: Good Question, so in the 20’s. The optimal is high 20’s from a surgeon standpoint. When you get up to 25, this is the normal BMI, as DIEP flap surgeons, we like when patients are a little bit heavier, it’s a little bit easier to get more volume obviously. However, I wouldn’t encourage gaining weight. I really avoid doing that at all costs just to make someone a candidate for surgery. Some people are happier at a slightly higher weight and that is just fine. It gets harder to do DIEP flaps when the BMI starts to get down towards 20. Most women can still get a DIEP flap with a BMI of 20, but a lot of it obviously depends on how you carry the tissue that you do have, and where it is on your body. Some ladies with a BMI of 21 that have had a couple of kids, and they’ve got a little pooch as they call it. I had a lady the other day that referred to it as a kangaroo pouch, which I hadn’t heard before but that works too. Anyway, some tissue that they wouldn’t mind getting rid of, if that is over the lower abdomen we can use it. Now ultimately, in addition to how you carry your tissue, another big factor is your breast size and what your expectations of final breast size are. Also, whether you will reconstruct in one breast or two. So a lady who is very thin, who needs one breast reconstructed who wants to keep the other to preserve sensation, or because the risk of the other breast is low, or what-have-you, in that situation we can use all the lower tummy for just the one breast. That’s often referred to as a stacked flap. But even ladies having bilateral procedures, so both breasts, can often have DIEP flap surgery even though a lot of surgeons will say “oh, you’re too thin.” Or “you’re not a candidate” it really does depend on how you carry your tissue. Even lower BMI patients, in the low 20’s can still be DIEP flap candidates. We see a lot of people in our practice who have been told elsewhere that they’re not a candidate for DIEP flap surgery for a variety of reasons. Previous abdominal surgeries, very few prevent DIEP flaps from being possible. Certain types of abdominal surgery, if you have had a previous full tummy tuck, you’re probably not going to be a DIEP flap candidate, or if you’ve had major abdominal reconstruction you probably won’t be a DIEP flap candidate. There is a couple of those that we’ve pulled off too, but it depends very much case-by-case. If you really feel that DIEP flap surgery is for your, and you definitely want to look into it, if you’ve been told you aren’t a good candidate; I strongly recommend a second opinion. A second opinion can never hurt, even if it’s just to confirm what your first opinion was, at least then you know. Please by all means hit us up for a second opinion. We are here for you. We see a lot of people and talk to a lot of people who want a second opinion. Please use the Virtual Consultation form if that’s something you feel would be helpful for you. The other thing about DIEP flap and BMI is we tend to push the envelope in terms of high BMI and that is based on work that came out of our practice. That is a study we did that was led by Dr. Ochoa. So we looked at complication rates, and we found that patients with a BMI of up to 40 are candidates for the procedure. Above 40 the complication rates really kind of start to take uptick. So the higher the BMI the higher the line goes (in an upward motion). The higher the BMI, the higher the risk of issues. When the BMI gets to 40, the line stops being a gradual increase and heads almost straight up. Now again, it depends on how you carry your weight. There are some ladies who have a BMI of less than 40 but the way they carry their weight; their risk will be more like a lady who has a BMI of over 40 so it is very much a case-by-case decision. This is the guide, so we really try to get our patients below 40 for DIEP flap surgery, it is just safer for you guys.
Question: What different platforms are you using for telemedicine and is insurance covering telemedicine?
Answer: We are using several platforms. At PRMA we pride ourselves on being very nimble and patient friendly, so we can do Skype, we can FaceTime. Those are the two most popular with our patients. We are able to do it in a way that we don’t document anything in either of those platforms, everything is documented straight into our EMR (electronic medical records) from a HIPPA protection standpoint. Skype and FaceTime are the most common platforms that we are using. Insurance is covering it, and last time I saw, but please confirm with your specific insurance carrier, co-pays and deductibles for telemedicine during this time were being waived. So Please do check with your individual insurance carriers and plans to make sure that is the case.
Question: Is PRMA taking care of billing insurance for telemedicine consults or is that the patient’s responsibility?
Answer: No, PRMA will take care of it. Virtual Consultations are very easy and very quick and we take care of billing your insurance.
Thank you guys for tuning in! If you would like more Facebook Live events to answer questions, or on certain topics, please get in touch and let us know what you would like us to cover. Everyone take care of yourself, stay at home, and stay safe. Thanks!
Author: Dr. Minas Chrysopoulo and Courtney Floyd
We understand the frustration and concern many patients seeking breast reconstruction are feeling during this time. Because of the COVID-19 outbreak, most reconstructive surgeries are being delayed for the safety of patients and to help conserve much needed PPE for healthcare workers on the front lines of fighting this virus.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

Breast Reconstruction Surgery and Your Period
Breast Reconstruction Surgery and Your Period December 02, 2020 Share on Facebook Twitter Linkedin During our pre-operative appointment with patients, a topic that occasionally arises is menstrual cycles. It is completely normal for women to experience changes with their periods throughout breast cancer treatments. These can be temporary or permanent. Periods can be unpredictable following […]

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap September 08, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]
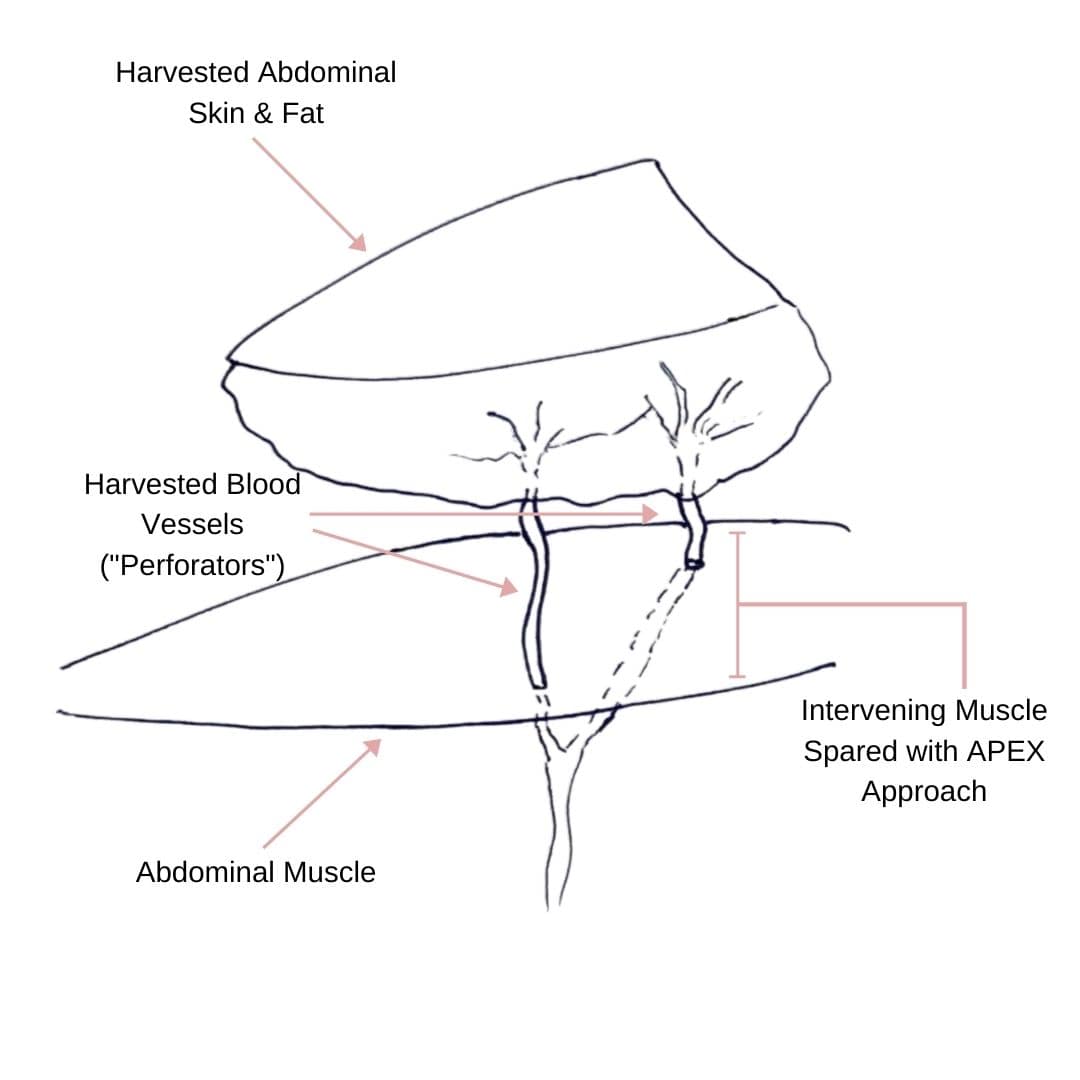
Comparing APEX Flap and DIEP Flap Breast Reconstruction
Comparing APEX Flap and DIEP Flap Breast Reconstruction August 10, 2020 Share on Facebook Twitter Linkedin We have been receiving numerous inquiries about the “APEX flap” recently. Patients want to know what it is and how it differs from the DIEP flap. APEX is an acronym that stands for “Abdominal Perforator Exchange”. Many patients believe […]
Monitoring the Health of Your Flap During & After Surgery
Monitoring the Health of Your Flap During & After Surgery July 21, 2020 Share on Facebook Twitter Linkedin Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap. During this procedure, surgeons transplant skin […]
COVID-19 and the Impact on Cancer Patient’s Mortality
COVID-19 and the Impact on Cancer Patient’s Mortality July 21, 2020 Share on Facebook Twitter Linkedin There is still so much we do not know about COVID-19. Likewise, there is little known about how this disease impacts mortality for cancer patients. A study published in The Lancet evaluated and characterized the outcomes of patients with cancer […]

No Comments