
Many women are going to have their therapeutic mastectomy in the absence of a reconstruction if they’re in a geographic area where reconstruction is having to be postponed because of the COVID-19 situation. What we’re going to do in our practice is make every effort to get those patients to their reconstruction as soon as possible. If we can do it in a matter of weeks or months, the tissues of the chest wall will be soft enough that they can accommodate a flap or an implant or whatever we [the patient and surgeon] choose to use. I think we can still get a really nice result. Obviously, an immediate reconstruction is optimal but there are going to be a great number of patients who don’t have that option and need to move forward with their mastectomies as soon as they can.
Is there something that you, as a surgeon, do in the OR in a ‘delayed’ setting that can help optimize the final result outcomes for flap and implant reconstruction patients?
We do a lot of delayed reconstruction as a matter of routine so we just recreate the defect on the chest wall expand the skin there as best a possible so that it will fill up nicely with soft tissue or implants. Patients could go our website and see examples of delayed reconstruction. We’re experienced in doing delayed reconstruction and again because of the situation we’ll probably have to do more of that than we ordinarily would. But again, we’ll get to those patients as soon as we can before the skins had a chance to sit down on the chest wall and contract and become less pliable.
In a situation where a patient has the option to place a tissue expander at the time of a mastectomy, is that a good option or would you recommend that in place of immediate reconstruction? What are the pros and cons?
That’s a great question and a controversial one. The benefit is you put the tissue expander in and it acts as a spacer – again in ‘plastic surgery speak’ this keep the skin out to length so that it retains that rounded or teardrop shape. That’s the pro. The con is tissue expanders have a known complication rate and so by putting in tissue expanders in everybody you may encumber complications like infection and exposure of the implant, fluid collections around the implant, etc. So, it solves one problem but can create others. In our geographic area placing a tissue expander is, for the most part right now, considered elective and to be postponed. There are some scattered exceptions to that. But in our practice we’ve decided not to do that because the Texas Medical Board has advised us not to do that and our local hospital wants us to preserve PPE (the materials that they might need to treat COVID patients). For that purpose we’ve decided not to put in tissue expanders.
What about women who are interested or are candidates for nipple sparing mastectomy? Is a nipple sparing mastectomy still an option even though they may to have to delay reconstruction during this time?
Another good question. Many of the general surgeons that we work with in our area will do a nipple sparing mastectomy in the setting of a delayed reconstruction. For example, a patient who is a candidate for nipple sparing mastectomy because of the location and size of the tumor but who needs post-operative chemotherapy, but more typically radiation therapy , maybe they have multiple positive axillary nodes or something…surgeons here will often do a nipple sparing mastectomy. The tissue sits down on the chest wall and then we come back and we do our delayed reconstruction as we would any of our usual delayed reconstruction. Patients in our area, patients coming from other states or other cities in Texas could certainly discuss that approach with their surgeons.
For women who really want to do immediate reconstruction at the time of their mastectomy, if it is clinically acceptable, would a lumpectomy be a better option to start cancer treatment and then follow later with the mastectomy and immediate reconstruction? And if so, what does that do to impact breast reconstruction results?
Yes, a very good point and it may be some women are a candidate to have a partial mastectomy or a lumpectomy to kind of tide them over if what they’re really seeking is a mastectomy. Then the majority of the breast is intact in the skin envelope over the breast and so that buys time. The acute cancer is out. That’s definitely a good option for a smaller tumor or the stage one tumor that’s in a favorable location. Then patients can come back and have a completion mastectomy and if needed a prophylactic mastectomy on the other side if there’s a family history or a genetic susceptibility component. That’s certainly one way that women can in essence get an immediate reconstruction.
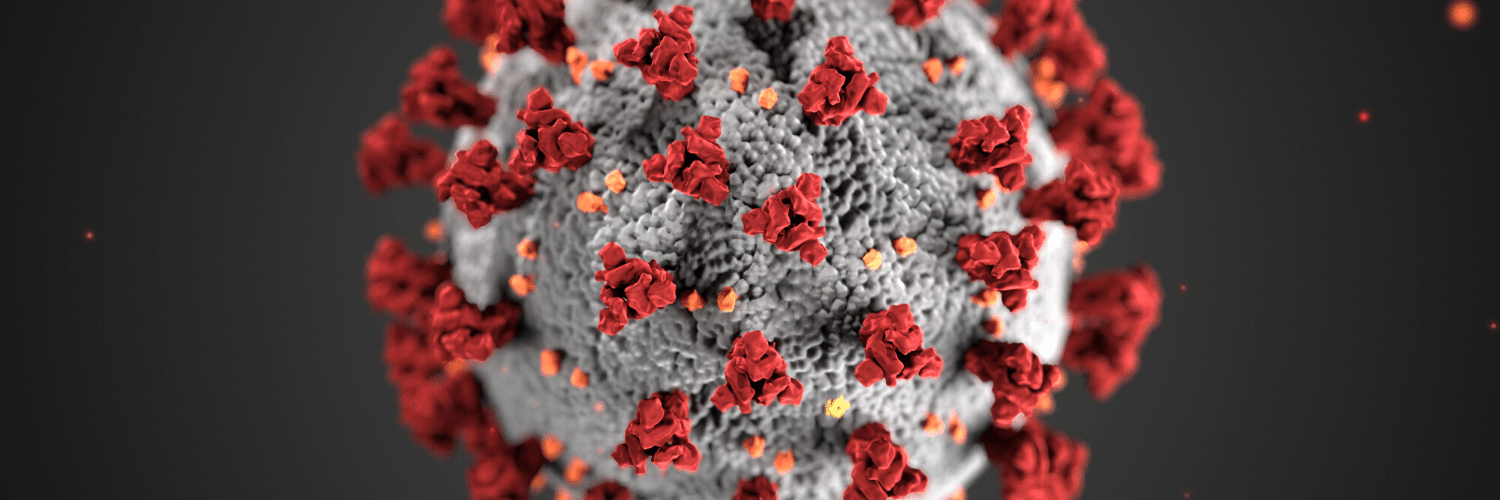
Can you give us some updates on specifically what’s happening in San Antonio as it relates to coronavirus outbreak and our efforts with keeping patients safe and our staff safe during this time?
As of this morning the San Antonio metropolitan health district has reported 503 cases in San Antonio. There has been unfortunately 12 fatalities. Overall San Antonio is behind the rest of the nation and we think that the peak of the curve is coming in the next week or so. So, San Antonio is in a favorable position relative to other parts of the country as it stands right now.
Author: Dr. Steven Pisano and Courtney Floyd
Many women are going to have their therapeutic mastectomy in the absence of a reconstruction if they’re in a geographic area where reconstruction is having to be postponed because of the COVID-19 situation






No Comments