Genetic testing is making a difference in risk management options for individuals who have an increased likelihood of developing breast cancer. For patients who elect to have genetic testing and find they carry one of the many gene mutations that increases the risk of breast cancer, prophylactic mastectomy is an option. This surgical risk-reduction approach involves removing the breast tissue – with or without sparing the nipple-areola – and can be followed by immediate breast reconstruction.
In a study published in Plastic and Reconstructive Surgery, genetic testing is now also recommended for breast cancer patients who choose to undergo a unilateral mastectomy with an abdominal based flap breast reconstruction procedure (like the DIEP flap).
The study followed 160 women with breast cancer who underwent a unilateral mastectomy followed by abdominal based flap breast reconstruction between 2007 and 2016. At an average follow-up of six years, three patients had been diagnosed with a second breast cancer in the originally unaffected breast. All three of these women proved to have a high-risk mutation that could have been detected by genetic testing before surgery.
Why is this important?
If these three women had known they were at high risk prior to their original mastectomy, they may have opted undergo a prophylactic mastectomy of the originally unaffected breast with bilateral reconstruction. This is because the abdominal based flaps can only be used once. If further mastectomy and reconstruction is necessary later, reconstruction would have to be performed using a breast implant or tissue from another area of the body.
“This study provides clear evidence that genetic testing is a must for women choosing unilateral (one sided) reconstruction,” says Dr. Chet Nastala. “Genetic testing can identify those patients who are at high risk for development of future cancers on the opposite breast which could have been prevented in hindsight. Although unilateral abdominal based reconstruction may be appropriate in select patients, this would not be the case if a genetic risk was identified beforehand. We would encourage all women to be fully aware of their genetic risk status as they plan their reconstruction.”
Author: Courtney Floyd and Dr. Chet Nastala
Genetic testing is making a difference in risk management options for individuals who have an increased likelihood of developing breast cancer.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading
Genetic Testing Before DIEP Flap Reconstruction – Is It Necessary?
Abdominal Tightness After DIEP Flap Surgery
Abdominal Tightness After DIEP Flap Surgery July 20, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction uses skin and fat from the lower abdomen to recreate a warm, soft, natural breast following a mastectomy. Because a portion of tummy tissue is removed and transplanted to the chest wall during this procedure, most patients experience […]

How Painful is DIEP Flap Breast Reconstruction?
How Painful is DIEP Flap Breast Reconstruction? July 20, 2020 Share on Facebook Twitter Linkedin When patients learn about DIEP flap as an option for breast reconstruction after a mastectomy, one of the first questions they ask is how painful the procedure is. The DIEP flap uses a patient’s skin and fat from the lower abdomen […]

Weight Changes and the Impact to DIEP Flap Breast Reconstruction Results
Weight Changes and the Impact to DIEP Flap Breast Reconstruction Results July 20, 2020 Share on Facebook Twitter Linkedin Will my reconstructed breasts change size if I gain or loose weight after DIEP flap surgery? We are often asked how future weight changes will impact final DIEP flap breast reconstruction results. The general answer is that your […]
Relationship Between BMI and Quality of Life after DIEP Flap Breast Reconstruction
Relationship Between BMI and Quality of Life after DIEP Flap Breast Reconstruction July 20, 2020 Share on Facebook Twitter Linkedin For many patients, breast reconstruction plays an important role in recovery after breast cancer treatment. Thanks to the introduction of the BREAST-Q (a patient reporting tool aimed to measure breast reconstruction results), patient reported outcomes […]

Options for Nipple Reconstruction after Mastectomy
Options for Nipple Reconstruction after Mastectomy July 20, 2020 Share on Facebook Twitter Linkedin Patients today have many choices to consider when faced with a breast cancer diagnosis. For patients who are not candidates for nipple-sparing mastectomy (or for those who choose not to save their nipples), nipple/areola reconstruction is an option. Nipple reconstruction can be performed in a […]
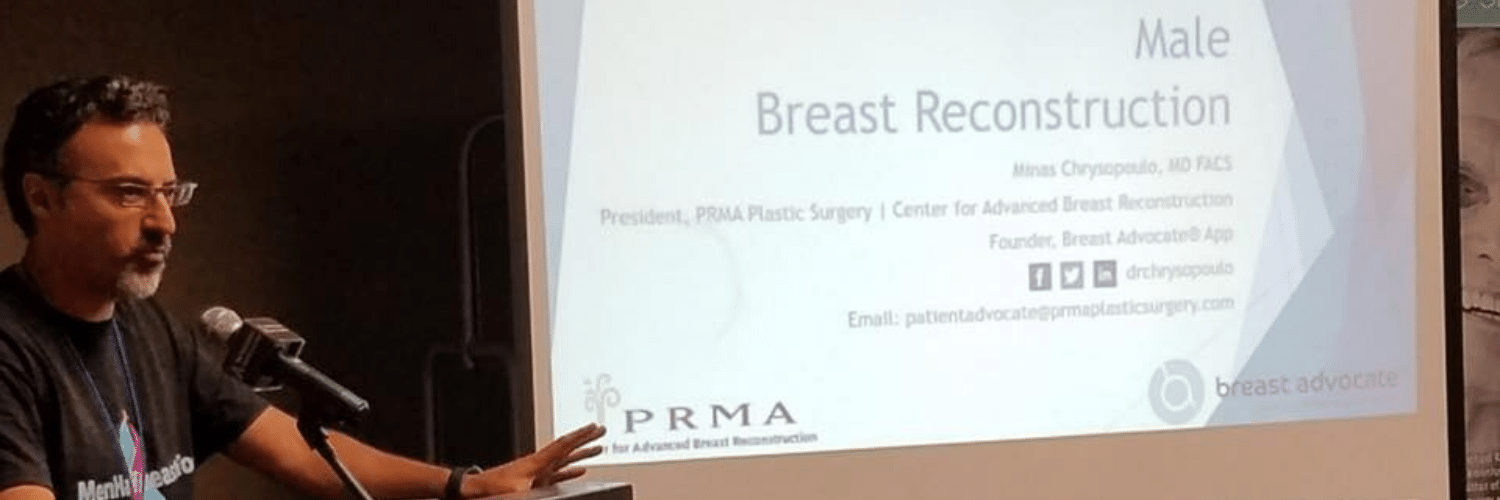
Male Breast Reconstruction Highlighted at Male Breast Cancer Coalition Meeting
Male Breast Reconstruction Highlighted at Male Breast Cancer Coalition Meeting July 20, 2020 Share on Facebook Twitter Linkedin This year, Dr. Minas Chrysopoulo, was joined the Male Breast Cancer Coalition (MBCC) at their annual conference to discuss male breast reconstruction options. “Like women, men can experience the same concerns about their appearance following breast cancer surgery,” […]

5 Reasons to Choose PRMA for DIEP Flap Reconstruction
5 Reasons to Choose PRMA for DIEP Flap Reconstruction July 20, 2020 Share on Facebook Twitter Linkedin PRMA Plastic Surgery is a world leading breast center specializing in today’s most advanced breast reconstruction techniques–like the DIEP flap. Here is why we believe you should choose PRMA for your DIEP flap surgery: 1) PRMA is one of […]

Choosing to Forgo Breast Reconstruction – “Going Flat”
Choosing to Forgo Breast Reconstruction – “Going Flat” July 20, 2020 Share on Facebook Twitter Linkedin Do you have to have breast reconstruction after a mastectomy? You do not! With every breast cancer diagnosis comes a plethora of decisions about treatment. One of those decision is whether to have breast reconstruction. There are many options […]
Study Finds At-Home 23andMe Genetic Test Not Reliable in Detecting Breast Cancer Risk
Study Finds At-Home 23andMe Genetic Test Not Reliable in Detecting Breast Cancer Risk July 20, 2020 Share on Facebook Twitter Linkedin The popular at-home genetic test 23andMe is making headlines again. Recent research presented at the American College of Medical Genetics and Genomics annual meeting showed the tests are not a reliable predictor of breast […]

No Comments