Author: Dr. Minas Chrysopoulo
“Do I still need to have mammograms after my breast reconstruction?” I’m asked this question quite often.
Surprisingly, there is no evidence-based consensus on this among breast cancer physicians. Recommendations range from “no need for any further mammograms” to “continued regular screening”.
Some doctors feel that since there is minimal natural breast tissue left behind after a mastectomy (it is impossible to remove all breast cells), there is no need to continue monitoring patients. Other surgeons decide on a patient-by-patient basis, including genetic predisposition (eg BRCA) and the type of reconstruction.
Though the risk is very low, breast cancer can return after a mastectomy. Breast reconstruction does not increase or decrease the risk of recurrence at all – the recurrence rate is the same whether women have reconstruction or not.
However, since the risk of breast cancer recurrence is a real one, I feel we need to continue some sort of monitoring once the reconstruction process is completed. This is especially the case in nipple-sparing mastectomy patients and patients who carry breast cancer associated gene mutations (eg BRCA).
Self breast exam is a no-brainer. It’s relatively easy to perform and it’s free.
For implant reconstruction patients it’s easier to feel changes in the skin against the underlying implant. Deep recurrences on the muscle (less common) are also theoretically easier to feel when the implant is placed under the muscle; the pectoralis muscle previously located under the breast tissue (ie at the “deep mastectomy margin”) is now displaced superficially and under the skin since it is pushed upwards by the implant placed beneath it.
For patients with silicone implants, the FDA recommends an MRI 3 years after the implants are placed followed by repeat MRIs every 2 years after that. This recommendation was provided when silicone im plants were re-introduced to the US market for cosmetic use as a means of checking implant integrity long-term. In the case of breast reconstruction, recurrent cancer is always going to be a more worrying concern for patients than documenting implant integrity. Ironically, when it comes to having the MRI covered by insurance, it is often easier to use the FDA recommendation as the underlying reason for having the test rather than trying to justify a screening test in a mastectomy patient with a benign clinical exam.
For women who are having an MRI to evaluate implant integrity, it is important to know an implant study is different to a “breast study” and does not detect cancer.
Generally speaking, I don’t personally feel routine MRIs are necessary but this approach is an option. While not as sensitive a test, ultrasound is a more cost effective alternative for screening, followed by MRI if the ultrasound shows something abnormal.
Patients who have had a flap reconstruction can also benefit from further imaging studies in addition to self exam.
The most commonly used breast imaging studies are mammograms and MRI. The appearance of a mammogram changes completely after autologous (flap) breast reconstruction. Even if the breast looks natural on the outside, the inside of the breast is completely different since the breast tissue has been replaced by fat (and sometimes muscle depending on the procedure) from another part of the body.
Some surgeons recommend flap patients have a one-off baseline mammogram, in essence a “flapogram”, after reconstruction just to get a new baseline. If the self breast exam reveals anything new of concern then the mammogram can be repeated, often in conjunction with an ultrasound for more information. Now the new mammogram can be compared to the baseline mammogram.
Another option is a one-off baseline MRI after breast reconstruction instead of a mammogram but this is a more expensive approach. MRIs are much more sensitive. Again, if self breast exam reveals a new area of concern in the future, the MRI can be repeated to see if anything has changed.
Some surgeons recommend continued screening mammograms after mastectomy and autologous (flap) breast reconstruction.
Flap reconstructions can develop areas of fat necrosis. This is fat in the reconstructed breast that becomes hard and creates a new mass which may or not be easily palpable on exam. A needle biopsy is often recommended to ensure the mass is benign and not a recurrence.
While the final recommendation on screening should be provided by the patient’s breast surgeon and medical oncologist, we feel that breast reconstruction patients should continue regular self-exams, especially if they have undergone a nipple-sparing mastectomy. For flap patients, a one-off baseline study once their reconstruction process is complete should also be considered. For some breast reconstruction patients, continued routine screening may be more prudent if their risk of future disease is high.
“Do I still need to have mammograms after my breast reconstruction?” I’m asked this question quite often.
Surprisingly, there is no evidence-based consensus on this amongst breast cancer physicians.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

Mammograms and MRI after Breast Reconstruction – Are They Needed?

Is there a Place For Breast Reconstruction in Metastatic Breast Cancer?
Is there a Place For Breast Reconstruction in Metastatic Breast Cancer? July 07, 2020 Share on Facebook Twitter Linkedin Author: Dr. Minas Chrysopoulo Can I still have Breast Reconstruction if I have Metastatic Breast Cancer? Traditional medical opinion states that patients with metastatic breast cancer are not candidates for breast reconstruction. Once metastases are diagnosed […]

Impact of Radiation on Breast Reconstruction Surgery
Impact of Radiation on Breast Reconstruction Surgery July 07, 2020 Share on Facebook Twitter Linkedin Author: Dr. Minas Chrysopoulo Can radiation therapy impact breast reconstruction results? Radiation therapy is often recommended as part of breast cancer treatment. Patients undergoing lumpectomy receive radiation routinely once they’ve healed from surgery. Some mastectomy patients also need radiation after […]
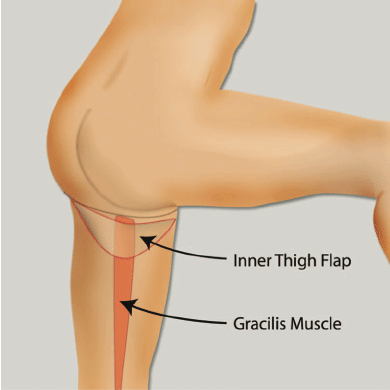
TUG Flap Restores Breast After Mastectomy With Thigh Lift Bonus
TUG Flap Restores Breast After Mastectomy With Thigh Lift Bonus July 07, 2020 Share on Facebook Twitter Linkedin What is TUG flap breast reconstruction? San Antonio, TX (PRWEB) February 23, 2009 – Plastic, Reconstructive & Microsurgical Associates (PRMA) of South Texas, a leading breast reconstruction surgery practice in San Antonio, is now offering women the […]
Breast Reconstruction after Mastectomy – Breast Reconstruction Specialist Radio Interview
Breast Reconstruction after Mastectomy – Breast Reconstruction Specialist Radio Interview July 07, 2020 Share on Facebook Twitter Linkedin What are the cutting edge breast reconstruction options currently available? It was an absolute pleasure to talk to DeLeon and Travis on “DeLeon Dialogue” last night. Breast cancer survivor DeLeon and cervical cancer survivor Travis talk frankly with […]

When Should You Consider Prophylactic Mastectomy of The Non-Cancer Breast?
When Should You Consider Prophylactic Mastectomy of The Non-Cancer Breast? July 07, 2020 Share on Facebook Twitter Linkedin When Should You Consider Prophylactic Mastectomy of The Non-Cancer Breast? Having breast cancer in one breast increases a woman’s chances of getting breast cancer in the second breast at some point. Unless the patient is “high risk” […]

Leslie Mouton’s Breast Reconstruction Diary
Leslie Mouton’s Breast Reconstruction Diary July 07, 2020 Share on Facebook Twitter Linkedin What’s it like to have breast reconstruction? PRMA Plastic Surgery would like to thank Mrs. Leslie Mouton, local news anchor for KSAT12 News in San Antonio, for documenting her experiences with breast cancer reconstruction. We hope that patients are able to gain […]

Cosmetic Surgery-Breast Procedures
Cosmetic Surgery-Breast Procedures July 07, 2020 Share on Facebook Twitter Linkedin What are the different cosmetic surgery options offered at PRMA Plastic Surgery? Our experienced surgeons offer breast augmentation (enhancement) with breast implants, breast lift (mastopexy), and breast reduction procedures. These procedures help create an aesthetically pleasing look for women who are self-conscious about their […]
Liposuction, Tummy Tuck (Abdominoplasty) & Body Lift
Liposuction, Tummy Tuck (Abdominoplasty) & Body Lift July 07, 2020 Share on Facebook Twitter Linkedin What are cosmetic surgery options to improved body contour? Patients seeking an improvement in body contour are usually candidates for either liposuction, a tummy tuck (abdominoplasty), a body lift, or some combination of these procedures. Our experienced plastic surgeons help […]
Microsurgical Breast Reconstruction With Perforator Flaps
Microsurgical Breast Reconstruction With Perforator Flaps July 07, 2020 Share on Facebook Twitter Linkedin What are perforator flaps? How are they used in breast reconstruction? Microsurgical breast reconstruction using perforator flaps represents the state of the art in reconstructive breast surgery after mastectomy. The tissue removed by the mastectomy is replaced with the patient’s own […]

No Comments