
How do PRMA surgeons monitor the health of a flap after breast reconstruction surgery?
Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap.
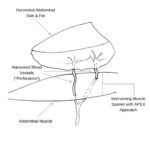
During this procedure, surgeons transplant skin and fat from the lower abdominal area (referred to as a “flap”) up to the breast area to recreate the breast mound. The blood vessels of the lower abdominal tissue flap are separated from their native location in the pelvis then reconnected to blood vessels in the chest using microsurgery. As the most critical portion of the procedure, the blood vessels are reconnected precisely during surgery facilitated by use of a high-powered microscope. Proper blood flow to the transplanted tissue is vital for the survival of the flap.
Blood flow to the tissue is closely monitored immediately following surgery to ensure the viability of the flap and to address/correct any complications as soon as possible. Although rare (occurring less than 1% of the time at PRMA), complications with blood flow can impact the survival of the flap, leading to a “failed reconstruction.”
Internally
Presurgical planning along with extensive training and proper surgical technique is critical in successfully performing autologous reconstruction. Reconnecting the flap to its new blood supply in the chest wall quickly and correctly is essential for the survival and health of the flap. While we (PRMA) perform all blood vessel connections by hand using conventional sutures, many microsurgeons incorporate the use of venous anastomotic couplers when performing autologous reconstruction. Venous couplers use two rings which connect to each other bringing the ends of the vessels together without the use of sutures. Studies have shown that using anastomotic coupler devices can reduce surgery time. However, in our experience, use of venous couplers have not promoted reduction in surgery times and can be associated with slightly higher rates of complications.
Externally
To monitor the health and viability of flaps immediately following surgery, both clinical examination and continuous external monitoring technology is used. In the post-operative period, our specialty-trained nursing staff performs detailed physical exams to verify continued blood flow to the tissue flap as well as monitor for signs of bleeding or other unforeseen events. In addition, external monitoring devices are placed on the skin surface of the flap during surgery in order to track and monitor tissue oxygen levels within the flap. Using external monitoring technology gives healthcare teams continuous real-time updates allowing the detection of any complications well before any symptoms become visible.
Addressing Complications
In the rare event the blood flow or sustainability of a new flap is in question, surgeons can act quickly to repair or adjust the blood flow to the flap. When a complication is identified, the patient is taken back into surgery immediately. Prompt return to the operating room will increase the probability of flap salvage without any long-term effects. While rare, “take back” surgeries typically do not impact the overall healing/recovery timeline for the patient.
Author: Dr. Oscar Ochoa and Courtney Floyd
In the rare event the blood flow or sustainability of a new flap is in question, surgeons can act quickly to repair or adjust the blood flow to the flap.
Leave Comment
No Comments







Lisa Campbell
I am considering PRMA for Allergen saline implant removal and hopefully DIEP reconstruction.
For patients traveling from out of state, how do you manage follow-up care especially with drains?
Also, my abdominal muscles have relaxed significantly due to seven full-per pregnancies – is it possible to
tighten those muscles during DIEP flap like you would for an abdomnioplastcy?
PRMA Plastic Surgery
Great questions Lisa! We would love to connect you with our dedicated out of state patient liaison who can walk you through how we care for our traveling patients.
Abdominal tightening is part of the DIEP procedure as well and our surgeons would be more than happy to answer any of your other questions! If you are interested in scheduling, please contact our office at 800-692-5565