Catch the replay of Dr. Chrysopoulo discussing sensory nerve reconstruction and how PRMA surgeons help to restore sensation back to a reconstructed breast following a mastectomy.
Can you explain to what causes the loss of sensation to the chest wall?
Yes, so when the mastectomy is performed, the breast surgeon removes all the tissue that looks and or feels like breast tissue. The nerves that come out of the chest to provide the feeling to the breast skin and to the nipple and the areola. There are several nerves, but unfortunately during the mastectomy it is very common for those nerves to be cut. So even though the breast surgeon is focused on removing just the breast tissue, sometimes, in fact most of the time, in most women, there isn’t a clearly defined change between breast tissue and the fat underneath the skin so it is very common to take a little bit of fat from underneath the skin with the breast tissue. So even though the nerves come out of the chest wall and travel in, for the most part, that subcutaneous fatty layer, it is very common for them to be damaged with mastectomies. So there have been a couple of reports in the media over the last couple of years that have really bashed reconstruction, in my opinion, because of the numbness that is associated with the process. What was missed in that conversation was the fact that it wasn’t the reconstruction that was leaving the patients numb. It was the mastectomy that causes the numbness in the first place. So the conversation should really be about how do we improve breast reconstruction further to include feeling rather than just what you see and touch. So adding that third dimension really. But the numbness is a factor of the mastectomy not the reconstruction, which is why women who “go flat” have numbness too, because the mastectomy causes it, not the reconstructions fault.
What steps are PRMA surgeons taking to help restore that lost sensation?
Before we get to that point, there is an extra step that we are taking, that I think is the most important, and that is the steps to preserve the feeling in the first place. So, some mastectomies are more aggressive than others, some breast surgeons are more aggressive than others in terms of removing tissue. We have to always remember and appreciate that the mastectomy is the most important aspect of a breast cancer patients care, and also the most important aspect for a high risk patient. So patients who have gene mutations, you can’t prioritize the reconstruction, you have got to prioritize removing everything that looks and feels like breast tissue, otherwise a patient isn’t getting the maximum benefit from the mastectomy in the first place. However, there are steps we can take during mastectomies to increase our chances of preserving those nerves that provide feeling in the first place. If that isn’t possible because of the patients’ anatomy, or because of the location of the breast cancer, then we take steps to at least identify the nerve in the first place and if we can at least preserve as much of it as we can in terms of its length. That makes reconstructing the nerve easier too. At PRMA we have been reconstructing nerves for many years, over a decade actually. I joined the practice I think, 15 years ago now, and we were doing nerve reconstructions back then. Our techniques now have increased, now we have nerve grafts, before we were only doing reconstruction of the nerves where the patients anatomy allowed us to reconstruct the nerve using only their own nerves. For example, with the DIEP flap, we would make sure to get a long nerve that supplied the skin to the lower abdomen, and we would take that nerve with the DIEP flap when we transferred it up to the chest, and we would connect that nerve to a nerve that we had identified at the time of the mastectomy, or after the mastectomy if it was a delayed patient and we would connect the two together. That is very successful, that is our primary technique still to this day, but there are some patients where you cannot get enough length on the nerve to allow you to connect the two nerves without a nerve graft. You need a bridging nerve graft to make up the gap sometimes. So, nerve grafts are now being used in our practice to bridge the gap when we can’t do what we call a primary nerve repair. So really at PRMA, does those three things to summarize. #1 preserve sensation as much as possible. #2 reconstruct the nerve where we can’t preserve it, there are two ways to reconstruct it, one using the patient’s own nerve tissue only, and the other technique is to use a nerve graft if you need to bridge a gap.
Can this be performed in both tissue reconstruction and implant reconstruction in patients? Or is it specifically for tissue reconstruction patients?
Well, not everyone is offering nerve reconstruction, so that is first and foremost. So irrespective of the reconstruction you are having most practices in the country still aren’t doing it. So that is number 1, you’ve got to find someone who is doing it. We have traditionally only done it in tissue reconstruction patients, so flap patients, not just DIEP flaps, you can also find a nerve in tissue that is being transferred from other parts of the body to the chest as well. So several types of flaps offer the ability to reconstruct a nerve as well, not just DIEP flaps. But now we are also looking at offering it in some cases for implant reconstruction cases. We haven’t started doing that yet, but it is only something that I am looking into. The insurance landscape is also something that we need to really evaluate and there are going to be instances where, and it has happened already, where the insurance plan doesn’t approve the nerve reconstruction. Thankfully in most cases it has been covered, but there have been some cases where patients have been disappointed where it hasn’t been covered, and that is something we also have to evaluate for our implant patients as well. We are getting there, but we need to cross that bridge still.
How long, typically, in your experience does it take for sensation to come back following sensory nerve reconstruction?
It takes nerves a millimeter a day to grow back, in most women, looking at several centimeters of regrowth. Women who have nerve reconstruction, if they needed a nerve graft, it will take longer because it is a longer distance for the new nerve cells to regenerate. Generally, I tell my patients you’ve got to give it several months, don’t pass judgement on whether it has worked or not for a year, and you may get improvement for up to two years. Obviously, we have had patients who have had the nerve reconstruction done, and who wake up and think I am an absolute genius because they still have all of their feeling, and the nerve reconstruction worked and ‘OMG Dr. C you are so amazing! I can feel everything already.’ You know, it is tough to burst their bubble, but unfortunately, it’s not my good work that is enabling them to feel their breast and nipple the day after surgery, those patients have benefited from preserving the nerves in the first place. There are obviously some instances where we are able to preserve nerves, and we also find a nerve that was cut, or another nerve that we can use to add to a nerve reconstruction too. So some people get preservation and a nerve reconstruction, it just depends on the patients’ anatomy, the cancer surgery that is being done, the breast surgery that is being done, and the breast surgeon that is involved. We are very lucky here in San Antonio, that we have great breast surgeons that are very eager and willing to try new things, and they have been very receptive to changing techniques to allow us to allow us to help them identify the nerves and to help them preserve the nerves. I am really very happy about the team we have here; our breast surgeons have been GREAT! If you are lucky enough to wake up with feeling, it’s not because of the nerve reconstruction that you have had, it’s because of the nerves that were able to be preserved.
How does breast sensation compare to a native breast when a patient has undergone sensory nerve reconstruction? Do they regain sensation everywhere on the breast, is it the same as mother nature provided?
So I tell my patients that every degree of sensation they might get back will be a bonus. So the only way to get close to the natural sensation is to preserve it in the first place. As we have said, that is not always possible, you’ve got to prioritize the patients’ care always it is life before breast. But If we manage to preserve the nerve, then that patient will have a very good chance of maintaining if not their natural sensation, something very close to it. It is very common for patients to have nerve preservation, but they still notice, initially at least, a significant change, but in those patients the sensation returns to normal quickly. If someone has lost feeling initially, and then a week later is it back, it is because the nerves were bruised or damaged but not cut. Again, you aren’t going to regain a ton of sensation from a nerve reconstruction after a week. The sensation you get back months and months later, that is the sensation you get back because of the nerve reconstruction. In patients’ in whom we can’t preserve the nerves, and who have no feeling, they get some feeling back because of the nerve reconstruction, it is very rarely going to be the same as mother nature. It is important for people to realize that, definitely beats the alternative of a numb breast but we are not at the point of restoring mother nature level of sensation. We still have a lot of questions that need to be answered, it is still very much an evolving field, and evolving technique. I know we have been doing it in primary reconstructions for a very long time but especially as nerve grafts are concerned we don’t know really which nerve is best. We think we have a good idea, but we don’t know how many nerve grafts are optimal, how many we should be performing in each breast, we don’t know what the ideal length of a nerve graft is necessarily. There are still lots of unanswered questions, thankfully we are a part of a big multi-center study right now that is ongoing, we are very excited about that. So over time we should have more answers to the long list of questions that we have. As always, the more you learn, the more questions you have. We have a long way to go.
What about patients who have had a Nipple Sparing Mastectomy, and also undergo the sensory nerve reconstruction. Is nipple sensation restored at all?
Women who have nipple sparing mastectomies tend to regain more feeling anyway. Even if you don’t do a nerve reconstruction. Some studies have looked at that, and preserving the nipple areola even if you don’t do nerve reconstruction it improves the quality of the sensation that comes back and can also improve the speed in which it comes back. That is a very important point, some nerve regeneration, especially with tissue reconstructions, especially with flaps, there is some degree of nerve regeneration anyway, even if you don’t do nerve reconstruction. What we are finding is that nerve reconstruction and nerve preservation improves the level of feeling further, beyond that. We feel very strongly that it is very worthwhile. Even women that don’t have any nerve reconstruction can regain some feeling. The big question for us in our practice is do you, and should you do a nerve reconstruction at all in someone that is having a nipple sparing mastectomy. Our approach is that you should still always prioritize nerve preservation. So the last thing we should be doing as reconstructive surgeons, as plastic surgeons, is cutting a nerve to be able to reconstruct it. In patients where we can preserve the nerve, and we can’t find a nerve that has been cut, we just won’t do a nerve reconstruction, if they have had nipple sparing. In a patient that has the nipple areola complex removed and we are doing a flap reconstruction and replacing the nipple areola with new skin that will later become the new nipple areola complex, then we try at all costs to do a nerve reconstruction in that case because you really want that skin that will in the future become the new nipple areola, you want that to regain as much sensation as possible. Again will it be like mother nature, no, but it is better than complete numbness. That is a great question about the nipple sparing, so really the bottom line is that it depends on the patient, it depends on the patients’ anatomy, depends on whether we are able to preserve the nerve, and if not it depends on whether we can identify a nerve that has been cut. We aren’t going to cut a nerve just to say we reconstructed it.
What about patients who choose to go flat, and still have that numbness across the chest, do they have any options for nerve reconstruction?
Not yet, good question though. To reconstruct a nerve, you have got to be able to identify nerves that have been cut. We have talked about identifying nerves as they come out of the chest, so that is where you plug the nerve graft into the identified cut nerve as it comes out of the chest, because that is the nerve that used to supply the breast. But now, in the case of someone who chooses to go flat, where do you plug that nerve graft into? So with a Nipple Sparing Mastectomy patient who has had a nerve cut, you know that the nerve graft has to connect the cut nerve as it comes out of the chest to a cut nerve that comes out of the nipple and areola if you can identify one. But with a patient who is choosing to go flat, where do you plug into? So that question, no one has really looked at as far as I know. The thing about patients who choose to go flat all of those nerve endings that have been cut are now on the chest wall will grow back into the mastectomy skin flaps that are now flat on the chest. So all of those nerves should grow into the tissue anyways, so over time someone who chooses to go flat should, just like a patient who has breast reconstruction who regains some feeling anyways, patients who choose to go flat should experience improved feeling over time. Like I said it is going to take a while, many months’ even up to a couple of years.
Learn more about sensory nerve reconstruction HERE.
Author: Dr. Minas Chrysopoulo and Courtney Floyd
We have to always remember and appreciate that the mastectomy is the most important aspect of a breast cancer patients care, and also the most important aspect for a high risk patient. So patients who have gene mutations, you can’t prioritize the reconstruction, you have got to prioritize removing everything that looks and feels like breast tissue, otherwise a patient isn’t getting the maximum benefit from the mastectomy in the first place. However, there are steps we can take during mastectomies to increase our chances of preserving those nerves that provide feeling in the first place.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

Breast Reconstruction Surgery and Your Period
Breast Reconstruction Surgery and Your Period December 02, 2020 Share on Facebook Twitter Linkedin During our pre-operative appointment with patients, a topic that occasionally arises is menstrual cycles. It is completely normal for women to experience changes with their periods throughout breast cancer treatments. These can be temporary or permanent. Periods can be unpredictable following […]

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap September 08, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]
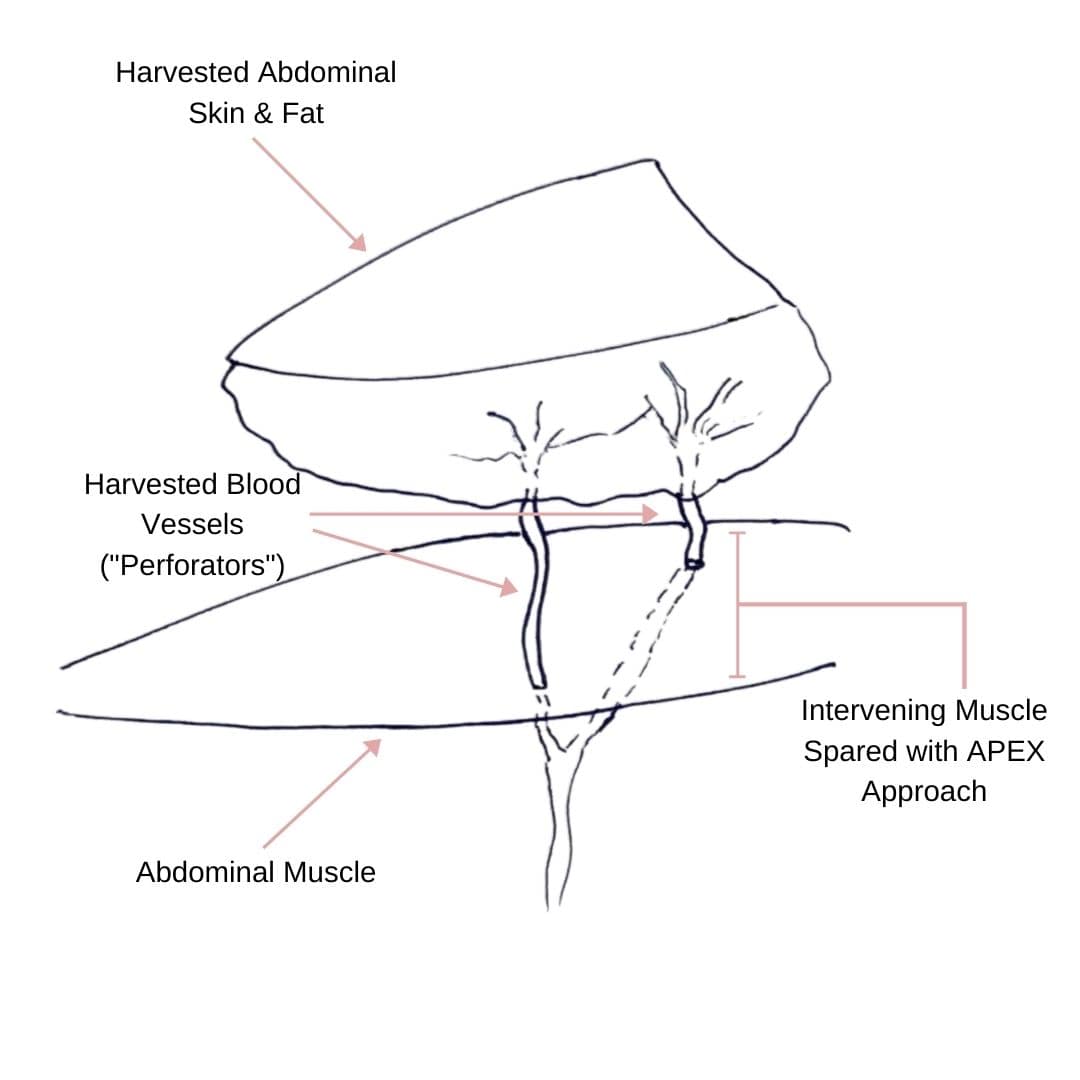
Comparing APEX Flap and DIEP Flap Breast Reconstruction
Comparing APEX Flap and DIEP Flap Breast Reconstruction August 10, 2020 Share on Facebook Twitter Linkedin We have been receiving numerous inquiries about the “APEX flap” recently. Patients want to know what it is and how it differs from the DIEP flap. APEX is an acronym that stands for “Abdominal Perforator Exchange”. Many patients believe […]
Monitoring the Health of Your Flap During & After Surgery
Monitoring the Health of Your Flap During & After Surgery July 21, 2020 Share on Facebook Twitter Linkedin Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap. During this procedure, surgeons transplant skin […]
COVID-19 and the Impact on Cancer Patient’s Mortality
COVID-19 and the Impact on Cancer Patient’s Mortality July 21, 2020 Share on Facebook Twitter Linkedin There is still so much we do not know about COVID-19. Likewise, there is little known about how this disease impacts mortality for cancer patients. A study published in The Lancet evaluated and characterized the outcomes of patients with cancer […]

No Comments