This week UT Southwestern Medical Center released a press release announcing their newest development in breast reconstruction techniques. The new method combines the advantages of two different types of microsurgical procedures using tummy tissue to reconstruct a breast after a mastectomy.
Wanting to know more I asked PRMA’s Dr. Oscar Ochoa to weigh in. Here is what he had to say:
“Abdominal-based flaps are widely regarded as the gold-standard in autologous reconstruction of the breast following mastectomy. With sparing of abdominal musculature and supporting fascia, deep inferior epigastric perforator (DIEP) and superficial inferior epigastric artery (SIEA) flaps have gained broad popularity due to maintenance of abdominal wall stability. While the abdominal tissue harvested with either DIEP or SIEA flaps is identical, the distinction between both flaps is determined by the vessels carrying blood to and from the flap tissue. The arteries and veins of DIEP flaps invariably match the recipient vessels in the chest wall making the vascular connections extremely reliable. On the other hand, the arteries and veins of SIEA flaps are generally of smaller diameter creating a mismatch when connected to the recipient vessels in the chest. The size mismatch makes performing the connections not only technically more difficult, but also potentially more risky as blood flow turbulence may precipitate formation of blood clots within the vessels disrupting blood flow to or from the flap. Although relatively rare (<5%), disruption of blood flow to the SIEA flap could ultimately lead to irreparable flap damage or failure.
Drs. Hallock and Teotia’s innovative solution to the size mismatch problem of the SIEA flap is meaningful! With this new technique, the deep inferior epigastric vessels (which are the source vessels of the DIEP flap) are sacrificed and function as an intermediary or graft between the SIEA flap and recipient chest vessels effectively minimizing the vessel size discrepancy seen with standard SIEA flaps thus theoretically decreasing the risk of blood clot formation due to flow turbulence. Two factors, however, require careful consideration prior to wide acceptance of this novel technique. First, utilization of the deep inferior epigastric vessels as an interposition graft between the SIEA and chest vessels is an intricate adjunct to an already complex procedure which will invariably add to the required operative and anesthesia time which in turn may increase complications. Second, the addition of the interposition vascular grafts increase the number of vessel connections (anastomoses) which is also known to increase the incidence of complications. Cumulatively, the detrimental effects of added operative time and increased number of anastomoses may offset the benefit gained by minimizing the vessel size discrepancy seen in standard SIEA flaps. Ultimately, clinical studies would be required to answer this intriguing question and determine the practical usefulness of this new technique.”
Overall, I believe the biggest take away from this new surgical technique is it is most certainly meaningful to the advancements in breast reconstruction using abdominal flaps, but should still undergo clinical studies to determine its usefulness. Great job UT Southwestern!
Author: Dr. Minas Chrysopoulo and Courtney Floyd
Overall, I believe the biggest take away from this new surgical technique is it is most certainly meaningful to the advancements in breast reconstruction using abdominal flaps, but should still undergo clinical studies to determine its usefulness.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

Hospital Stay After DIEP Flap Breast Reconstruction: What to Expect
Hospital Stay After DIEP Flap Breast Reconstruction: What to Expect December 09, 2020 Share on Facebook Twitter Linkedin Following DIEP flap breast reconstruction, patients are typically in the hospital for about 2-3 days. During that time, patients often wonder what they should expect. Here is what a typical hospital stay for PRMA patients entails… Flap […]

Breast Reconstruction Surgery and Your Period
Breast Reconstruction Surgery and Your Period December 02, 2020 Share on Facebook Twitter Linkedin During our pre-operative appointment with patients, a topic that occasionally arises is menstrual cycles. It is completely normal for women to experience changes with their periods throughout breast cancer treatments. These can be temporary or permanent. Periods can be unpredictable following […]

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap October 22, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]
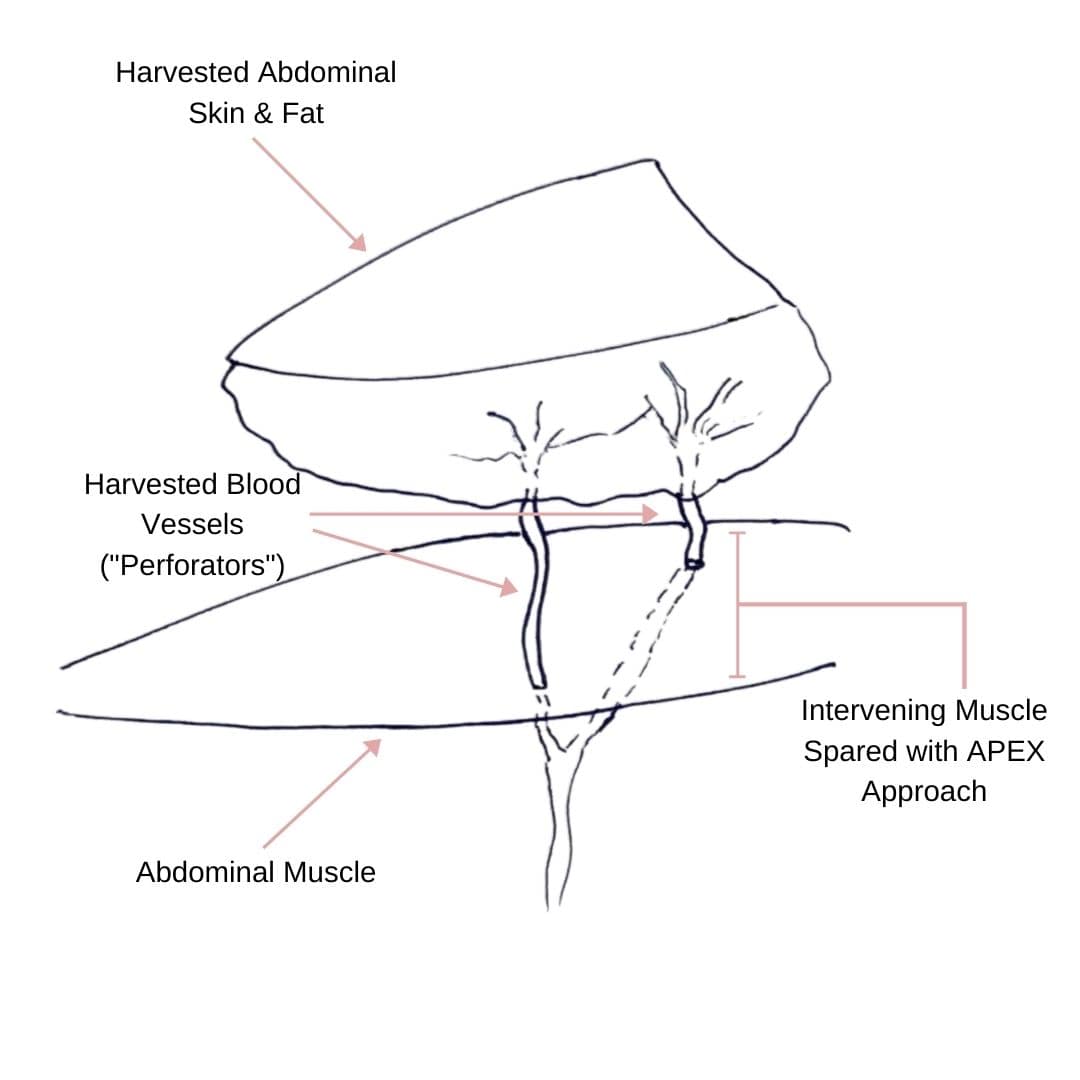
Comparing APEX Flap and DIEP Flap Breast Reconstruction
Comparing APEX Flap and DIEP Flap Breast Reconstruction August 10, 2020 Share on Facebook Twitter Linkedin We have been receiving numerous inquiries about the “APEX flap” recently. Patients want to know what it is and how it differs from the DIEP flap. APEX is an acronym that stands for “Abdominal Perforator Exchange”. Many patients believe […]
Monitoring the Health of Your Flap During & After Surgery
Monitoring the Health of Your Flap During & After Surgery July 21, 2020 Share on Facebook Twitter Linkedin Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap. During this procedure, surgeons transplant skin […]

No Comments