
Author: Dr. Minas Chrysopoulo
Can you grow new breasts from fat stem cells for breast reconstruction after a mastectomy?
A new form of breast reconstruction that allows women to grow new breasts from their own fat cells after a mastectomy could be offered to British and Australian breast cancer patients for the first time in 2010.
A human trial of the new technique¬ is being planned by plastic surgeons at a London hospital. The trial will study whether fat cells can be induced to multiply and fill a breast-shaped mold implanted under the chest skin to recreate a breast after mastectomy. Australian scientists also recently announced that they would start similar treatments on women within six months, following animal studies involving mice and pigs that successfully re-grew breasts from fat.
If the human trials are as successful, this new technique could transform breast reconstruction surgery, offering an alternative to breast implant reconstruction and more complex tissue transfer techniques requiring signicant down-time.
The technique is expected to take about eight months to grow a breast. Initially it will only be used to reconstruct breast cancer patients who have been cancer-free for at least 2 years. Eventually it may also be used for cosmetic breast augmentation allowing women to achieve a significantly larger breast size without needing saline or silicone implants.
The Australian team is led by Professor Wayne Morrison of the Bernard O’Brien Institute of Microsurgery in Melbourne. After a decade or so of working on this project he has now obtained ethical approval for a trial involving a handful of women.
I had the pleasure of listening to a presentation by Dr Morrison at the American Society for Reconstructive Microsurgery in 2008. The technique involves using liposuction to remove some of the woman’s own fat cells. The concentration of stem cells within this fat is then boosted in the laboratory. A biocompatible scaffold is then implanted under the patient’s skin, to create a cavity that matches the shape of her remaining, natural breast. The stem cell-enhanced fat solution is then injected into the scaffold. Over time, the scaffold is filled by the multiplying fat cells which obtain the necessary nutrients from blood vessels surgically wrapped around the scaffold.
The first trials will likely require that the scaffold is removed at the end of the reconstruction process though there is some talk of making the scaffold absorbable in the future so this extra step can be avoided.
Right now the focus remains on growing a breast made completely of fat, without breast glandular tissue, milk ducts or nipple-areolar tissue. The nipple and areola will therefore still need to be reconstructed as an additional step.
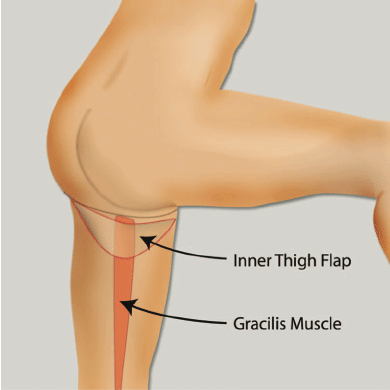
These developments are very exciting. I am sure this is the direction breast reconstruction is going in. The most advanced techniques currently available, like the DIEP flap for instance, already use the patient’s own fat to recreate a very natural breast. In the case of the DIEP flap, this tissue (fat and skin) is taken from the lower abdomen, providing the benefit of a tummy-tuck at the same time.
While DIEP flap breast reconstruction only takes a few hours (as opposed to eight months), it does involve major surgery and the creation of scars on another part of the body (lower abdomen). In addition, women still need a second surgery for “fine tuning” and nipple reconstruction. In essence then, the reconstruction process can still be fairly drawn out and take several months. I am sure many women will be eager to avoid major surgery and scarring for what could be a very similar end result once this new technique is optimized.
A new form of breast reconstruction that allows women to grow new breasts from their own fat cells after a mastectomy could be offered to British and Australian breast cancer patients for the first time in 2010.










No Comments