
- 4 Comments
- PRMA Plastic Surgery
July 08, 2020
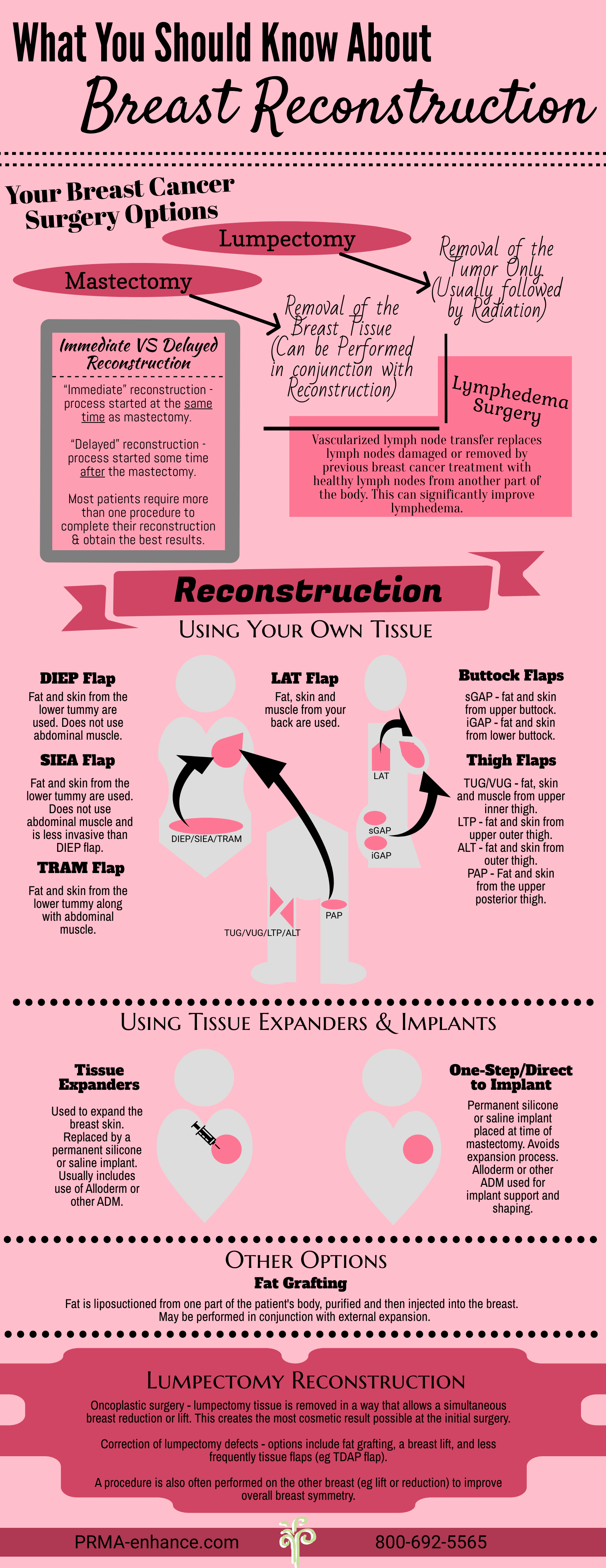
What are your breast reconstruction options after a lumpectomy or mastectomy?
Breast reconstruction makes women physically whole again after breast cancer. It restores something that nature provided but cancer has taken away. In the US, it is covered by insurance thanks to a 1998 Federal Mandate.
Unfortunately, many breast cancer patients are not offered the option of breast reconstruction after mastectomy or lumpectomy.
Women have several reconstructive options regardless of the type of breast cancer surgery being performed. After a mastectomy, options range from implants to “flap” techniques which use the patient’s own tissue to recreate a “natural”, warm, soft breast. Breast reconstruction can also be performed at the same time as a lumpectomy to maximize the cosmetic results and maintain breast symmetry. This is known as “Oncoplastic surgery”.
PRMA is one of the leading breast reconstruction practices in the World. We are very experienced with all types of reconstructive breast surgery, but do have a strong focus on state-of-the-art microsurgical procedures using the patient’s own tissue. This is because these procedures generally provide superior and much more “natural” results long-term than implants. Flap procedures are also strongly recommended instead of implants if the patient has had or will be having radiation.
Immediate vs. Delayed Breast Reconstruction
These terms define when the reconstructive process begins.
Immediate reconstruction is performed at the same time as the mastectomy and provides the best cosmetic results. Advantages include keeping the natural breast skin (“skin sparing mastectomy”) and less scarring. In some cases nipple-sparing mastectomy can be performed; this preserves the nipple and areola as well as the breast skin.
Immediate reconstruction enables the patient to wake up from the surgery “complete” and avoid the experience of a flat chest. Most women with early breast cancer (stage I or II) are candidates.
Delayed reconstruction usually takes place several months after the mastectomy. Patients having radiation may be advised to delay the surgery for the best results. This delay may be for several months. This allows the chest tissues to heal as much as possible after the radiation. Other reasons for delaying reconstruction include advanced disease (stage III or IV) and lack of access to a reconstructive surgeon.
Whether the reconstructive process is started at the time of the mastectomy (“immediate”) or some time after (“delayed’), it important for patients to realize that in most cases, further surgery is required to complete the reconstructive process and achieve the best cosmetic results.
Breast Reconstruction Options
1. Tissue Expanders and Breast Implant Reconstruction
This is the most common method of reconstructive breast surgery currently being used in the United States. Most surgeons perform implant reconstruction as a two-stage procedure. The tissue expander is essentially a temporary breast implant which can be placed either at the same time as the mastectomy or after the mastectomy has healed. The expander is used to stretch the skin envelope and recreate the size of breast the patient wants. The expander is ultimately replaced by a permanent implant (saline or silicone) at a separate procedure several months later.
Some patients undergoing immediate breast reconstruction are candidates for direct-to-implant reconstruction whereby the permanent implant is inserted at the time of the mastectomy and the patient avoids going through the whole expansion process.
An acellular dermal matrix (ADM), such as Alloderm, is a biological sheet-like material which is also used in most implant reconstructions. The ADM is used inside the breast and is not visible. When the implant is placed under the pectoralis muscle, the ADM covers the lower part of the implant that is not covered by muscle. It also acts as a sling to help secure the implant in position. When the implant is placed on top of the muscle (known as the “pre-pec” technique), the ADM is used as a wrap or drape over the implant, which provides an extra layer of coverage over the implant under the skin.
There are many opinions regarding types of implants and it is advised that you speak with your surgeon as to which implant would be best for you. Patients who undergo implant reconstruction should be aware that their breast implants may need to be replaced at a future date. Implants are also associated with a higher risk of complications than tissue flaps in the setting of radiation.
2. Muscle Flaps
Latissimus Dorsi Flap
The latissimus flap uses muscle from the back of the shoulder blade which is brought around to the breast mound to help create a new breast. During the procedure a section of skin, fat and muscle is detached from the back and brought to the breast area.
Many patients also need a tissue expander placed under the muscle in order to obtain a satisfactory result. The expander is replaced by a permanent implant at a second procedure down the line. Patients will have a scar on their back shoulder region that can sometimes be seen through a tank top, swimsuit or sundress.
Women who are very active in sports should know that this procedure may reduce the ability to participate in activities like golf, climbing, swimming, or tennis.
TRAM (Transverse Rectus Abdominis Myocutaneous Flap)
The TRAM flap was the first procedure to describe use of one of the rectus abdominis muscles (sit-up muscles) for breast reconstruction. This procedure begins with an incision from hip to hip rather like a “tummy-tuck”.
A flap” of skin, fat and one of the patient’s abdominal muscles is typically tunneled under the skin to the chest to create a new breast. This is known as a pedicled TRAM flap. Recovery from the TRAM flap procedure can be difficult and painful and there is a risk of abdominal bulging (or “pooching”) and even a hernia. Long-term, the patient has to adapt to the loss of some abdominal strength (up to 20%) which some active patients may notice.
In cases where both breasts are being reconstructed, both abdominal muscles are sacrificed and transferred to the chest (one for each breast). The loss of abdominal strength in these situations is far greater and very significant.
Over the years and with the introduction of microsurgery, the procedure has evolved several times with each modification preserving more and more abdominal muscle. This has made postoperative recovery a little easier and has decreased the potential for abdominal complications somewhat. The TRAM flap is still widely performed by plastic surgeons, but is very rarely performed at PRMA due to the muscle sacrifice involved.
3. Perforator Flaps
PRMA specializes in perforator flap breast reconstruction. These procedures use skin and fat from various parts of the body while preserving the patient’s muscles. Since no muscle is sacrificed recovery is much easier and muscle strength and function are preserved long-term. The downside to these procedures is that they are technically much more demanding than other breast reconstruction techniques and require microsurgical expertise. For this reason they are not offered by many plastic surgeons and patients must be prepared to travel when choosing these procedures.
The most common types of perforator flaps include:
DIEP (Deep Inferior Epigastric Perforator) Flap
The DIEP flap is the latest evolution of the TRAM flap and represents today’s gold standard in breast reconstruction. The DIEP flap procedure is similar to the TRAM flap but only requires the removal of skin and fat. Unlike the TRAM flap, the DIEP preserves all the patient’s abdominal muscle.
The blood vessels required to keep the tissue alive lay just beneath the abdominal muscle. Therefore, a small incision is made in the abdominal muscle in order to dissect the vessels and microsurgery is required to reattach the blood vessels to the chest area. Even though an incision is made in the abdominal muscle, NO abdominal muscle is removed or transferred to the breast in the DIEP flap procedure. As a result, patients do not have to sacrifice their abdominal strength and they experience less pain and a much quicker recovery. The risk of abdominal bulging and hernia is also very small in experienced hands.
The DIEP flap was first described in the early 1990’s but was slow to gain popularity, presumably because of the increased complexity and difficulty of the procedure compared to the TRAM.
The advantages of the DIEP flap are multiple: it uses living tissue to recreate a breast that often looks and feels like a normal breast; abdominal strength is not affected; the risk of bulging or hernias is significantly reduced; and, like the TRAM flap, the patient benefits from a simultaneous “tummy-tuck”, though unlike the procedure performed strictly for cosmetic reasons, the final abdominal scar can end up a little higher.
SIEA (Superficial Inferior Epigastric Artery) Flap
The SIEA flap procedure is very similar to the DIEP flap procedure. The main difference between the SIEA and DIEP is the artery used for blood flow supply to the reconstructed breast. The SIEA arteries are generally found in the fatty tissue just below skin. As in the DIEP the SIEA flap reconstruction does not sacrifice the abdominal muscle and only uses the patient’s skin and fat to reconstruct the breast. While the SIEA flap procedure is similar to the DIEP it is used less frequently since less than 20 % of patients have the anatomy required to allow this procedure.
GAP (Gluteal Artery Perforator Flap)
GAP Women who do not have an adequate amount of abdominal tissue for reconstruction may be eligible for the GAP flap. This procedure uses excess skin and fat from the upper or lower gluteal or buttock region. Fat and skin from either the upper or lower buttock region can be used and microsurgically transplanted to the chest.
Again, no muscle is sacrificed. Incisions can generally be hidden by most underwear. If a patient requires a bilateral reconstruction with GAP flaps many surgeons prefer to only perform one side at a time. It is important to discuss this possibility with your surgeon.
Thigh Flaps
Like the GAP flap, various thigh flaps are an option in cases where there is not enough lower abdominal tissue to reconstruct the breast(s). The TUG (Transverse Upper Gracilis) flap uses tissue from the upper part of the inner thigh; the PAP flap uses tissue from the upper posterior thigh just below the buttock crease, and the LTP flap uses tissue from the saddle bag area.
Once again, these procedures are not widely available due to their complexity and need for microsurgical expertise.
4. Fat Grafting
Fat grafting (also known as “lipofilling”) is commonly used in conjunction with other breast reconstruction techniques or after a lumpectomy to optimize breast contour and improve the final cosmetic results. Some surgeons advocate using fat grafting on its own to reconstruct the entire breast. The procedure involves liposuctioning fat from one part of the patient’s body, purifying it and then injected into the breast.
There are several fat grafting techniques that are used by plastic surgeons. Regardless of the fat grafting technique used, some of the injected fat will be reabsorbed over time (most studies quote reabsorption rates between 30% and 50%), but this can vary depending on the exact clinical situation and technique used. Patients must therefore be prepared to require more than one procedure for the best results. Reconstructing an entire breast requires multiple procedures.
Several independent studies have evaluated breast cancer patients over several years after lipofilling and concluded that fat grafting is oncologically safe in mastectomy patients and does not increase the risk of breast cancer recurrence.
5. Oncoplastic Surgery
Oncoplastic surgery is breast reconstruction performed at the same time as a lumpectomy.
In many cases, a lumpectomy can leave a significant breast deformity. This deformity is often made worse by the radiation therapy that typically follows a lumpectomy. During an oncoplastic procedure, the lumpectomy tissue is removed in a way that allows the plastic surgeon to perform a simultaneous breast reduction or lift. This avoids unwanted cosmetic deformities and simultaneously creates the most cosmetic result possible.
Most patients usually also need a breast reduction or lift of the other breast to achieve the closest breast symmetry. This is usually performed at the same time as the oncoplastic surgery.
Good candidates for oncoplastic breast surgery include:
- larger breasted patients
- patients who have tumors located away from the nipple/areola
- patients who have only one tumor. (Patients who have more than one cancer in different parts of the breast, known as “multi-centric disease”, are not good candidates)
Patients with small breasts (A or B cup) are not usually candidates for oncoplastic surgery as they typically do not have enough breast tissue left behind after the lumpectomy to rearrange into a cosmetically appearing breast. Correcting the lumpectomy defect in an acceptable way can be impossible in small breasted patients. These women are therefore often better served by a mastectomy and immediate breast reconstruction for the best cosmetic results.
As with breast reconstruction after a mastectomy, oncoplastic surgery is usually best performed by a breast surgeon-plastic surgeon team experienced in these procedures.
6. Lumpectomy Reconstruction
If oncoplastic surgery was not performed for any reason, lumpectomy reconstruction can also be performed after completion of all breast cancer treatment.
The most common technique is fat grafting. For larger contour defects of the outer and central breast, a flap, usually from the back, can be used. These flaps have traditionally used a small latissimus flap. Newer techniques preserve the back muscle and transfer only some of the overlying skin and fat (eg TDAP flap, ICAP flap). These flaps are best suited to reconstruct lumpectomy defects of the outer part of the breast.
Flaps from other parts of the body that are usually used reserved for reconstruction after a mastectomy are also occasionally used after a lumpectomy. These are only used for very significant lumpectomy defects, and for defects on the inner part of the breast.
Author: Dr. Minas Chrysopoulo
Breast reconstruction makes women whole again after breast cancer. It restores something that nature provided but cancer has taken away. It is covered by insurance thanks to a 1998 Federal Mandate.
Leave Comment

Have had tummy tuck and incisional hernia repair (upper abs) before having left masectomy.
Not interested in TRAM. What would be other options?Sheri Turner
July 17,2020

Great question Sheri! Because of your surgical history you would not be a good candidate for the TRAM or the DIEP flap, but there are other flap reconstruction options that you may be a candidate for (such as the GAP or TUG).
PRMA Plastic Surgery
July 17,2020

I have had multiple surgeries to reconstruct breast and each surgery is not successful. What are my options both breast look visibly different.
Renee
July 17,2020

So sorry to hear you are going through this Renee! Depending on your current circumstances, there could be many options available to you.
For personalized recommendations from one of our surgeons you can fill out our FREE virtual consultation form at https://prma-enhance.com/schedule-a-consultation/
PRMA Plastic Surgery
July 17,2020
Sign Up for Our Monthly Newsletter
Continue Reading
A Year in Review at PRMA – 2020
A Year in Review at PRMA – 2020 December 28, 2020 Share on Facebook Twitter Linkedin The COVID-19 global pandemic is an event that has made 2020 a year like no other. It can be hard to feel optimistic or reflect on the good with a year full of unprecedented change. “This past year has […]

Reducing the Risk of Chronic Opioid Use After Breast Reconstruction with ERAS Protocol
Reducing the Risk of Chronic Opioid Use After Breast Reconstruction with ERAS Protocol December 16, 2020 Share on Facebook Twitter Linkedin A study presented at the 2020 San Antonio Breast Cancer Symposium reported that women with breast cancer may be at a high risk of developing a chronic opioid addiction following mastectomy and reconstructive surgery. […]

Hospital Stay After DIEP Flap Breast Reconstruction: What to Expect
Hospital Stay After DIEP Flap Breast Reconstruction: What to Expect December 09, 2020 Share on Facebook Twitter Linkedin Following DIEP flap breast reconstruction, patients are typically in the hospital for about 2-3 days. During that time, patients often wonder what they should expect. Here is what a typical hospital stay for PRMA patients entails… Flap […]

Breast Reconstruction Surgery and Your Period
Breast Reconstruction Surgery and Your Period December 02, 2020 Share on Facebook Twitter Linkedin During our pre-operative appointment with patients, a topic that occasionally arises is menstrual cycles. It is completely normal for women to experience changes with their periods throughout breast cancer treatments. These can be temporary or permanent. Periods can be unpredictable following […]

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap October 22, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]

Growing New Breasts from Fat Stem Cells: Fact or Fiction? Is this the Future of Breast Reconstruction
Breast Reconstruction: Reconstructive Options After Mastectomy

Sheri Turner
Have had tummy tuck and incisional hernia repair (upper abs) before having left masectomy.
Not interested in TRAM. What would be other options?
PRMA Plastic Surgery
Great question Sheri! Because of your surgical history you would not be a good candidate for the TRAM or the DIEP flap, but there are other flap reconstruction options that you may be a candidate for (such as the GAP or TUG).
Renee
I have had multiple surgeries to reconstruct breast and each surgery is not successful. What are my options both breast look visibly different.
PRMA Plastic Surgery
So sorry to hear you are going through this Renee! Depending on your current circumstances, there could be many options available to you.
For personalized recommendations from one of our surgeons you can fill out our FREE virtual consultation form at https://prma-enhance.com/schedule-a-consultation/