- 2 Comments
- PRMA Plastic Surgery
The fields of breast cancer and breast reconstruction research have made incredible strides over recent years. New advances in chemotherapy agents, genetics, and surgical management of advanced breast cancer continue to change the landscape of treatment on a regular basis. Similarly, breast reconstruction research continues to significantly contribute to better patient outcomes following mastectomy. Despite recent advances, many unanswered questions remain requiring continuous multifaceted efforts in order to provide patients with optimal results.
As nationally recognized leaders in breast reconstruction, PRMA is actively involved in various components of breast reconstruction research spanning both clinical and basic science fields. In an effort to better characterize our broad involvement in ongoing research, a brief overview of a few of our current initiatives are presented:
Re-excision of residual cancer following mastectomy and reconstruction – In a small percentage of women undergoing mastectomy for breast cancer or pre-malignant lesions, residual cancer cells may be left behind at the previous location of the lesion(s). Unfortunately, this is not usually discovered until thorough evaluation by a pathologist is completed a few days later. Treatment of this residual cancer is controversial, especially after breast reconstruction has been performed immediately following mastectomy. One option is radiation to the reconstructed breast in an effort to “kill off” any residual cancer cells. Naturally, radiation can lead to unwanted short and long-term complications. PRMA promotes an alternative option where patients undergo an additional surgical procedure where the residual cancer cells are directly excised. Outcomes following this unique re-excision procedure related to reconstruction complications, cosmetic outcome, and most importantly, cancer recurrence are being submitted for publication.
Patient-reported outcomes following breast reconstruction – As reconstructive surgeons, our ultimate goal is to facilitate a patient’s recovery from breast cancer. By providing patients with a sense of “wholeness” through breast reconstruction, patients are less likely to experience a lingering sense of loss, depression, or anxiety in social or intimate situations. Through standardized questionnaires given to patients before and after surgery, PRMA has been able to identify specific factors such as age, body mass index, patient ethnicity, and others that are associated with obtaining a successful result from a patient’s point of view. After all, shouldn’t success in breast reconstruction be defined by the patients themselves?
Extended lymph node evaluation – Determination of whether breast cancer has spread to surrounding lymph nodes is a critical component of proper breast cancer treatment by helping to accurately establish the “stage” of the breast cancer. Based on the breast cancer stage, chemotherapy and/or radiation may be recommended in order to decrease the possibility of recurrence of cancer and increase survival. Evaluation of lymph nodes in the axilla has long been considered the standard-of-care in determining lymph node involvement with breast cancer. Although 25% of breast tissue drains into lymph nodes located along the breast bone (aka sternum) beneath the ribs, these nodes are difficult to access and are thus not routinely biopsied, potentially leaving involved lymph nodes unaccounted for and inaccurately staging patients.
In the majority of breast reconstruction surgeries that involve replacing the removed breast with the patient’s own tissue from the abdomen, thigh, or buttock area, these lymph node along the sternum are exposed and biopsied by PRMA physicians. If cancer is identified in these lymph nodes, more accurate staging is established that may lead to changes in their cancer treatments. PRMA is involved in determining whether these changes in cancer staging translate into improved outcomes and prolonged survival.
Radiation to the breast after immediate breast reconstruction – Breast reconstruction at the same time of mastectomy (immediate breast reconstruction) is currently recommended only in early stage breast cancer (cancer < 5cm in diameter, < 4 lymph nodes involved). If the breast cancer is diagnosed at an advanced stage and will require radiation even after mastectomy, reconstruction is not performed immediately but delayed until a later time (delayed breast reconstruction), which eliminates the psychosocial benefits of immediate reconstruction. Delaying the reconstruction until radiation is completed theoretically decreases radiation injury to the flap of tissue used to reconstruct the breast. This dogma was established many years ago when radiation delivery techniques were rudimentary and very imprecise. Since that time, radiation delivery techniques have advanced significantly allowing only the target tissue to be treated with radiation while sparing adjacent harmless tissue such as the reconstruction flap.
Although PRMA still adheres to these recommendations, some of our patients have undergone immediate breast reconstruction with subsequent recommendations to receive radiation due to a larger-than-expected cancer or numerous involved lymph nodes identified after mastectomy. PRMA is currently performing studies that evaluate the radiation-induced complications that are experienced by these unique patients on the side of radiation compared to non-radiated reconstructed breasts. It is possible that due to advancements in radiation delivery techniques, radiated reconstructed breasts may have a similar complication profile than non-radiated breast reconstructions. If true, immediate breast reconstruction could now be offered to patients with advanced breast cancer eliminating the need for delayed breast reconstruction.
Vascularized lymph node transfer– Upper extremity lymphedema is a tremendously debilitating complication of breast cancer treatment due to axillary lymph node removal. The affected limb becomes swollen impairing function due to lack of lymphatic fluid drainage. At PRMA, patients with lymphedema are treated with an adjunct procedure at the time of breast reconstruction where lymph nodes, normally located in the groin area, are transferred (en bloc) with the abdominal tissue into the affected axilla. With addition of groin lymph nodes into the affected axilla, re-establishment of lymph drainage may be promoted alleviating swelling and improving function. We are currently evaluating the objective benefit (and possible complications) of such lymph node transfer procedures.
Genetic mutations promoting hereditary breast cancer – The fields of molecular biology and genetics have contributed significantly to our current understanding of breast cancer. With identification of mutations in certain genes, lifetime risk of development of breast cancer in affected individuals is as high as 90%. Young women that are diagnosed with one of these genetic mutations are often undergoing preventative mastectomies in order to eliminate the possibility of developing breast cancer in the future.
Our current understanding as to how these genetic mutations predispose an individual to develop breast cancer is still lacking. PRMA is collaborating with UT Health Science Center San Antonio in a joint investigation utilizing the latest molecular techniques on PRMA patient tissue samples in order to better elucidate the mechanism involved in the development of breast cancer.
Author: Dr. Minas Chrysopoulo and Courtney Floyd
The fields of breast cancer and breast reconstruction research have made incredible strides over recent years. New advances in chemotherapy agents, genetics, and surgical management of advanced breast cancer continue to change the landscape of treatment on a regular basis. Similarly, breast reconstruction research continues to significantly contribute to better patient outcomes following mastectomy. Despite recent advances, many unanswered questions remain requiring continuous multifaceted efforts in order to provide patients with optimal results.
Leave Comment

This is why PRMA is a leading center for breast reconstruction. The research, shared information and consideration of patient outcomes makes them well-deserving of their reputation. I speak from the standpoint of a more than satisfied patient. Thank you to all the docs for their dedication and hard work.
Terri
July 20,2020

Breast reconstruction is more than just about the surgery, it includes everything that comes with. PRMA is excellent at connecting the pieces to provide a well-rounded outcome. I am extremely grateful.
Stanlie
July 20,2020
Sign Up for Our Monthly Newsletter
Continue Reading

Hospital Stay After DIEP Flap Breast Reconstruction: What to Expect
Hospital Stay After DIEP Flap Breast Reconstruction: What to Expect December 09, 2020 Share on Facebook Twitter Linkedin Following DIEP flap breast reconstruction, patients are typically in the hospital for about 2-3 days. During that time, patients often wonder what they should expect. Here is what a typical hospital stay for PRMA patients entails… Flap […]

Breast Reconstruction Surgery and Your Period
Breast Reconstruction Surgery and Your Period December 02, 2020 Share on Facebook Twitter Linkedin During our pre-operative appointment with patients, a topic that occasionally arises is menstrual cycles. It is completely normal for women to experience changes with their periods throughout breast cancer treatments. These can be temporary or permanent. Periods can be unpredictable following […]

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap October 22, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]
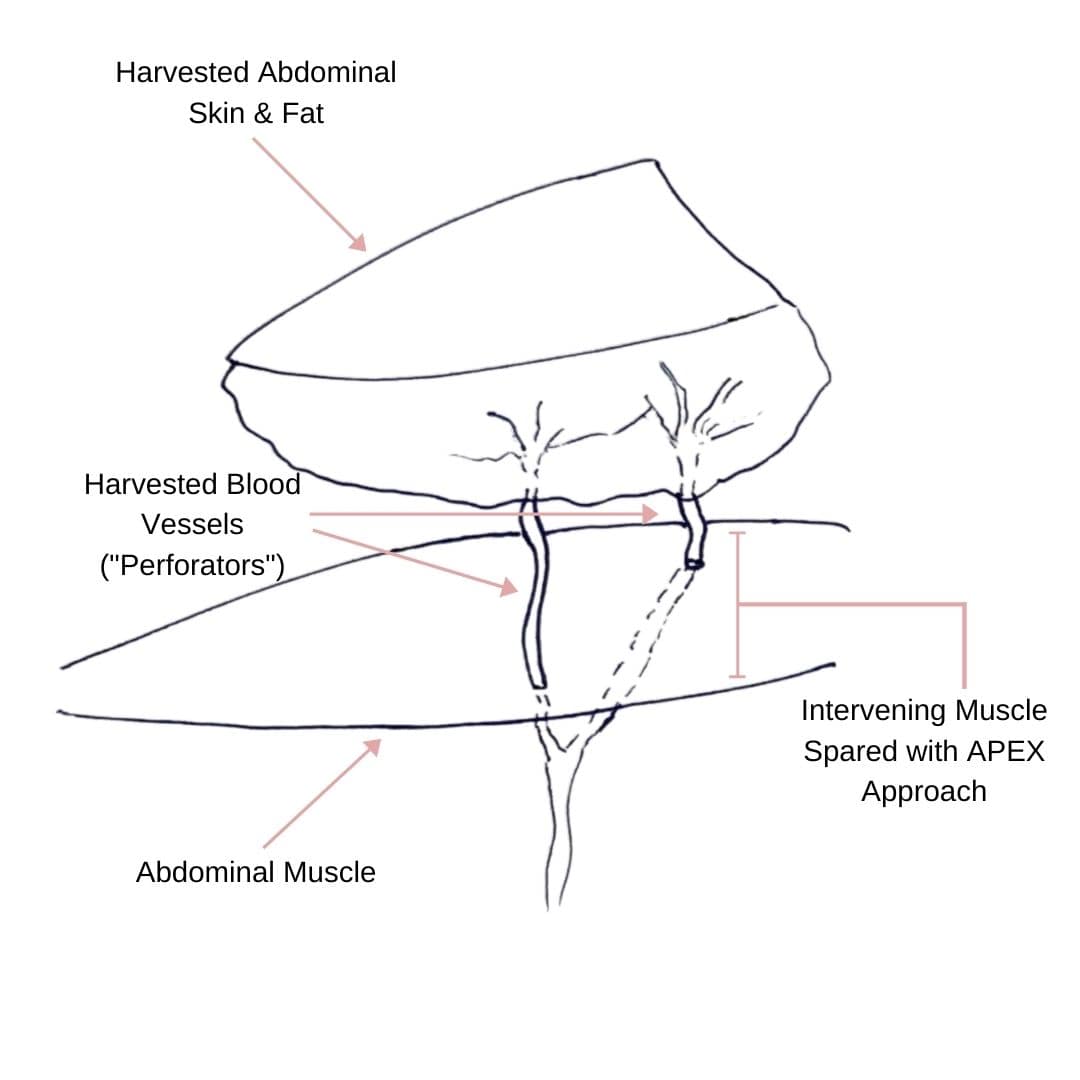
Comparing APEX Flap and DIEP Flap Breast Reconstruction
Comparing APEX Flap and DIEP Flap Breast Reconstruction August 10, 2020 Share on Facebook Twitter Linkedin We have been receiving numerous inquiries about the “APEX flap” recently. Patients want to know what it is and how it differs from the DIEP flap. APEX is an acronym that stands for “Abdominal Perforator Exchange”. Many patients believe […]
Monitoring the Health of Your Flap During & After Surgery
Monitoring the Health of Your Flap During & After Surgery July 21, 2020 Share on Facebook Twitter Linkedin Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap. During this procedure, surgeons transplant skin […]

Stage Two Breast Reconstruction Surgery (Revision Stage)
The Great Mammogram Debate

Terri
This is why PRMA is a leading center for breast reconstruction. The research, shared information and consideration of patient outcomes makes them well-deserving of their reputation. I speak from the standpoint of a more than satisfied patient. Thank you to all the docs for their dedication and hard work.
Stanlie
Breast reconstruction is more than just about the surgery, it includes everything that comes with. PRMA is excellent at connecting the pieces to provide a well-rounded outcome. I am extremely grateful.