
Author: Dr. Gary Arishita
Is implant breast reconstruction safe after radiation therapy?
It is estimated that in 2013, more then 232,000 women will be diagnosed with invasive breast cancer with over 64,000 being diagnosed with in-situ disease. Of these women, half will be treated with lumpectomy and radiation treatments.
Radiation is an essential part of treatment for some women. Risk of recurrence and death can be significantly reduced with radiation in women undergoing lumpectomy. In locally advanced breast cancers, radiation can also be necessary after mastectomy.
Radiation works by damaging cellular DNA. Cells that are rapidly dividing are damaged more by radiation than normal cells. The beneficial effects of radiation following lumpectomy have been well proven. In the vast majority of cases, lumpectomy is not an acceptable treatment for breast cancer unless radiation is added as the breast cancer recurrence rate is too high after lumpectomy alone.
Radiation has deleterious effects on normal breast tissue as well. The radiation causes permanent changes to the normal breast tissue. It causes fibrosis of the tissues and decreases elasticity. The breast feels tighter and the skin and underlying tissues are less “stretchy”. The microvascular circulation is damaged and blood flow is reduced. These effects are present in the breast and skin forever. The changes can be more pronounced in some patients, but all treated tissues are affected.
Radiation increases the risk of complications and poor outcomes in breast reconstruction. When tissue expander and implant reconstruction is used after radiation, major complications occur in about half of patients. A major complication usually means that more surgery was needed and the implant had to be removed. It is then more difficult to perform reconstruction in tissues that have been scarred by infection or wound breakdown in addition to the radiation. Some plastic surgeons offer implant reconstruction to patients that have been previously treated with radiation. They cite data showing that it can sometimes work. The early results can sometimes appear good but less than half of patients will have an acceptable reconstruction long-term.
I do not recommend attempting tissue expander or implant reconstruction in patients who have been previously treated with radiation. I believe that a 50% complication rate is too risky. If the reconstruction fails, it is even more difficult to get a great result. I recommend that a tissue flap be used for reconstruction following radiation. When transplanting healthy, non-irradiated tissue to the breast, the flap behaves more like normal tissues and the health of the surrounding tissues improves significantly.
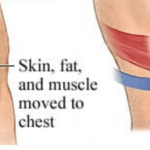
Tissue can be taken as a flap from the abdomen, the back, the buttock, or the thigh. Often the reconstruction can be made entirely of transplanted flap tissues. In patients who do not have enough tissue available, I use a combination of a flap along with a tissue expander or implant. The addition of the healthy flap to the radiated breast improves the overall health of the tissues and allows use of implants. Healing is improved and the cosmetic appearance of the breast is better when a flap is used along with an implant.
There are always choices in treatment. This applies to cancer treatment as well as reconstruction. I strongly recommend looking at your options and the short and long term impact of those treatment choices.
I hope this helps.
It is estimated that in 2013, more then 232,000 women will be diagnosed with invasive breast cancer with over 64,000 being diagnosed with in-situ disease. Of these women, half will be treated with lumpectomy and radiation treatments.
Leave Comment
No Comments






Robin
I sure wish someone had told me this. I am now dealing with nothing but a hard lump and one breast is higher than the other one. And this is after 2 surgeries. One to put the implant in and one to try to correct it by removing the implant and simply putting in a new one. He told me to push down on it to make it more level with the other breast.
PRMA Plastic Surgery
Hi Robin, PRMA routinely performs corrective surgery on patients who are unhappy with a previous breast reconstruction. I would be happy to talk about your options. You can give me a call at 800.692.5565 and if you’d like to complete our virtual consultation form, one of our surgeons can review your case and give you a better idea of what he would recommend. You can find that form via this link—> https://prma-enhance.com/schedule-your-consultation/. Hope to talk with you soon! -Brandy
Tracy
I wish I had been told this, as well Robin. I’ve had 2 surgeries as well and am looking at 1 or 2 more….that I know of so far and this process is taking a great deal of time. I don’t dare push down on my right implant because my scar hasn’t fully healed from when it broke open after a friend hugged me in March 2013. I’m saddened by all this and am tired of feeling discomfort and/or severe pain for close to 1 year. I don’t feel like a survivor, yet I still have hope.
Sheila
Hi Tracey and robin I agree I am having the same problem with implant failure after radiation, I am going in for my fifth surgery tomorrow, I wish someone would have explained that the tram flap was the recommendation
Dr. Arishita
I am surprised to see how often implants are used in women after radiation treatments. In my residency, I was taught that it usually did not work. The use of ADMs (Acellular Dermal Matrix) has helped to decrease capsular contracture. I think that has encouraged some surgeons to attempt implant reconstructions in radiated tissues. It does work sometimes. But, I have seen too many patients with bad results, so I do not attempt to reconstruct radiated breasts with implants. I don’t believe it is the best way to do it. Fortunately, I belong to a group, PRMA where I am able to offer all methods of breast reconstruction to my patients. I believe that I always offer the best option for my patient. The options are not limited to only those operations that I can perform. For women who have had poor outcomes after reconstruction, there is usually something that can be done to make it better. Usually it does require surgery. And it may require a more involved procedure, but the choice is yours. Dr A
Beverly
I underwent a mastectomy last June in Italy, followed by chemotherapy. 4 weeks after finishing chemo finished I had an implant put in before starting my radiation. I started radiation 4 weeks after the reconstruction ( 25 sessions). My silicone implant is now smaller and harder (more ball shaped). My plastic surgeon wants to inject fat around it to correct the shape. I am not happy with the feel of the implant. What do you think my options are?
PRMA Plastic Surgery
Hey Beverly! The implants reaction to the radiation is a normal response. Fat grafting is always an available option for you to help improve the shape and feel. However, due to the tightness of your skin after radiation, the transferred fat could likely reabsorb. You may want to consider an autologous reconstruction such as a DIEP flap or even LAT flap with the addition to the implant for a better shape and softer feel.
Dawn
I’ve had lumpectomies and radiation treatments back in 2012, had a bilateral mastectomy done in sept of 2013. Just in march of 2014 had an emergency surgery to remove the left implant and now I have only one breast that has the expander in it. My surgeon is gonna take the fat from my belly to put in it’s place when I get surgery again. My breast size is like a large B … He is saying there isn’t enough fat to make it the same size and the radiated skin is the problem as well. I don’t want to go thru all that pain and look like a boy. I’m going through all this alone, I have no husband or kids. I just want to be normal again. Now I also have lymph edema in my left arm. What do I do??? I’m sadden with all of this … 2 years too long
PRMA Plastic Surgery
Hey Dawn, I am so sorry to hear you are experiencing so many complications! PRMA routinely performs corrective surgery on patients who have had failed implant reconstruction. Our surgeons also perform vascularized lymph node transfer surgery, which can sometimes help with lymphedema. I would love to talk about your options. You can give me a call at 800.692.5565 and if you’d like to complete our virtual consultation form, one of our surgeons can review your case and give you a better idea of what he would recommend. You can find that form via this link—> https://prma-enhance.com/schedule-your-consultation/. Hope to talk with you soon! -Courtney
Donna
Hi Dr. A… I have read this article, and the comments. Thanks for posting this, I am looking forward to meeting you Friday, and see what your recommendations are for me. Feeling every confidence in you. Donna
PRMA Plastic Surgery
Hey Joanna! It is understandable that you are feeling confused and uncomfortable with your reconstruction. PRMA does perform corrective breast reconstruction and we would be happy to review your case. You can fill our our virtual consultation at https://prma-enhance.com/schedule-your-consultation/. After I receive your information, I can forward it onto our physicians to review. If you have any questions, please give me a call at 800-692-5565. Thanks, Courtney
Joanna
I have had breast implants since age 27. Age 31 I was diagnosed, had a lumpectomy with reexcision, chemo, and radiation. I soon developed a capsullary contracture after. I consulted a military doctor who was not comfortable with reconstruction to irradiated breast but offered fat grafting to the surgical site. I am now 34 and really dissatisfied having one breast that sits much higher than my healthy breast. I recently went back to the original plastic surgeon who did my implants to begin with and he felt reconstruction was safe at this point and would include doing a capsullectomy, replacing the implant and adding an ADM. He indicated this would require use of an expander (which after reading your recommendations sounds very concerning) and wanted to create a flap on my side near the affected breast to cover and improve the aesthetics of the scarring and surgical site. I am very confused at this point about my treatment options.
Sonia
Hello I was diagnosed in 2010 and had chemo and radiation done in 2011. I didn’t loose much of my breast. I had a small lumpectomy. I always wanted to do breast argumentation and now I’m going to have implants. My doctor told me of the risk and also told me that the implants under the muscle and fat grafting under the skin would be the way do do my breast implants. He will do both at same time, fat grafting only on the breast I had radiation. My breast look that had radiation looks normal and soft. I understand the damage us inside but do you think the risk of implants is reduced when it’s done under muscle and with fat grafting? Thank you
PRMA Plastic Surgery
Hey Sonia! Vast majority of implant based breast reconstruction is performed by placing the implant under the muscle, so your risk would likely remain the same. Fat grafting will be beneficial in achieving symmetry and correcting any unwanted irregularities in the shape of the breast. Let us know if you have any other questions!—Courtney
Kamila
Hi everyone, I don’t even know where to begin! Well July 26th, 2013 I had a lumpectomy and lymph node dissection, 4 days later it was confirmed I was pregnant. I kept the pregnancy and started chemo on October 7th, 2013, had the baby prematurely on March 12 with one more chemo to go. Around April 10th I started radiation treatment on still swollen breasts even though I didn’t breast feed. Now, my right breast (Cancer side) which used to be smaller, is bigger than left. I lost a lot of weight with treatment but my right affected breast somehow froze in time, it stayed a little bigger and firm (very painful too) while the rest of my body shrank. I am 36, 5’9” and weigh now 126 lbs. I am sad about the way I look, angry at this situation and afraid that I’ll never be able to look even again. I don’t know what to do. I thought the cancer breast would look considerably smaller after treatment, but it just got harder and size didn’t change from right after giving birth. Sorry for the long story, I am just sad. Thank you!
PRMA Plastic Surgery
Sweet Kamila, I am so sorry you have had to endure such a struggle! Side effects of your radiation are likely to blame for your “situation.” Please know there are many options for reconstruction available to you. PRMA routinely performs delayed breast reconstruction on patients who have had radiation. Please feel free to contact me at 800-692-5565 or patientadvocate@prmaplasticsurgery.com and we can work on setting you up with a consultation. Thanks—Courtney
janet swartz
30 years after radiation i had bil mastectomy with tissue expanders. 7 days post op the radiated side looks horrific purple grey blistered skin peeling off w the drain after 3 days was draining thick grey green liquid without an odor which was making everyone happy but me. red swollen very painful
getting worse rather than better.
the drain just slipped out of radiated side after four days and now at post op day nine i wake up covered in the thick drainage from breast incision not getting any better incision looks horrible can’t even really identify it anymore
what should i do now???? help
PRMA Plastic Surgery
Hi Sweet Janet!
I am so sorry to hear of all you’ve been going through. You may need to have a serious conversation with your plastic surgeon about keep in vs. taking out the expander on your radiated side before any more damage is done. Obviously it is not ideal or fun to think about going back to surgery so soon, but it may be worth it to get their opinion going on what course of action will help you heal better without possible infections and wounds. Whatever can be done to preserve your skin may be your best option and once you’re healed an autologous flap reconstruction might be your best option for reconstruction. Unfortunately the complication rate is higher on radiated skin and tissue to have expander and implant reconstruction vs. autologous flap reconstruction such as DIEP flap and other flaps utilizing your own tissue.
Lee
I recieved implants in November 2006, then was diagnosed with BC in my left breast in April 2014. At that time, I had a lumpectomy and 6 weeks of radiation. Now just a few months later, in Janurary 2015, My left breast has moved upward on my cheast and become hard and painful. I reached out to my original plastic surgeon and we discussed capsulotomy and/or capsulectomy while leaving the implant in (if still in good condition if not replacing it). I am worried about my options and this might not ‘fix’ the problem or that it will reoccur and I will be back on the table in a few years or even worse months. Is there anyway to tell?
PRMA Plastic Surgery
Hello Lee! Unfortunately, there is no way to tell if complications could reoccur over time. One thing I might recommend is looking into having a free flap based surgery such as the DIEP flap in place of your implants. You can find more information about these procedures under the breast reconstruction tab on our website. I am always available to answer questions at 800-692-5565. Thanks, Courtney Floyd—PRMA patient liaison
Kirstyn
Hi there, I live in Sydney Australia and have been trolling the interenet looking for info on Anaplastic Large Cell Lymphoma. I am 43 yrs and first had saline implants in my early 20’s. Went on to have 2 pregnancies, no trouble with implants. Early 2010 my right implant ruptured and I had both replaced with silicone implants. My surgeon at the time, though reputable, mistakenly replaced my round implants with shaped implants (significantly different results). He also removed too much tissue in one area which left a distinct bony region on my chest wall. He exchanged the implants for a much larger size 240cc to 550cc to fill in the area without my knowledge. The result was hideous. I had surgery with another surgeon who did beautiful work and performed full lift, reduction down to 240cc. I then developed a staph infection and had the left implant removed for 6 months and then replaced. 12 months later my right breast started to swell with seroma fluid. Had a full exchange February this year, however the problem continued in the same breast. I have since been diagnosed with ALCL and been advised to have both implants removed and that they cannot be replaced. I am aware that this is a rare condition with only 6 reported cases in here Australia and in the region of 70 worldwide with very little information. I have been told that my results of the seroma testing showed an extremely light reading and only a very mild dose of radiation would be required. I am considering trying the radiation with the implants in situ and would appreciate any thoughts or feed back you may have. Many thanks
PRMA Plastic Surgery
Indeed ALCL is an extremely rare complication of breast implants. Essentially, chemotherapy and radiation are likely necessary to treat the condition. It is advisable that, at the very least, the affected implant AND capsule be removed. The contralateral side implant may or may not need to be removed. The capsule surrounding the implant is the location that harbors the malignant cells and MUST be removed. The patient may elect to keep the implant (with the capsule) in situ in the setting of radiation treatments, but the radiation will not be effective in preventing a recurrence of the disease. In addition, radiation will ultimately cause capsular contracture and the implant will eventually have to be removed due to cosmetic complications. If, after implant removal and radiation is complete, the patient needs additional volume to the radiated breast, autologous reconstruction could be performed. Hope this helps.
Popylove
Why can’t capsular contracture be corrected by removing the implant and replacing with a new one? I had chemo, mastectomy with immediate reconstruction (implant using ti-loop) then radiotherapy. My skin seems to have stuck to the implant and the Breast/implant has shrunk and hardened. The skin looks perfectly healthy and soft.
PRMA Plastic Surgery
Capsular contracture can be corrected temporarily by removing part of or the entire capsule and placing a smaller implant; however, due to the long-lasting effects of radiation, the risk of contracture and migration of the implant is high. Tissue that has been radiated tends to tighten over time (no matter if it has been days, weeks or even years since the last treatment). This causes the implant to shift upward on the chest, moving to where it has least resistance, and oftentimes causing the capsule to contract.
Staci
This is exactly my worry! I also received implants in 2006. Just had my lumpectomy and am supposed to start radiation now. What was your outcome and how are you doing? smile
PRMA Plastic Surgery
Hello Staci! If you do experience adverse side effects after radiation therapy, you may consider replacing the implants with a tissue flap breast reconstruction such as the DIEP flap. It is always best to consult with a board certified plastic surgeon. You are more than welcome to fill out our virtual consultation form and one of our surgeon can provide you with recommendations.
Maureen
I’ve had two lumpectomyies followed with a Mastectomy and now facing the beginning of chemo on the 29th My surgeon and Chemo Dr said I would not need radiation and I am going thru reconstruction of the breast with an expander in me now – then the radiation Dr now says she advises radiation also for 6 weeks due to the most recent studies. My tumor was not 5 cm but I did have 2 positive lymph nodes out of 11 that were removed. I do not want problems with the reconstruction plastic surgery and plan to talk with my chemo Dr again but I don’t believe I need the radiation in addition to chemo. Please respond with advice if you are knowledgeable. Thank you.
PRMA Plastic Surgery
Good morning Maureen. It is best for you to follow the advise of your treating cancer physicians. Your health comes first and reconstruction comes second. If you are worried about complications with implants and radiation, you may want to consider a flap based reconstruction surgery. You can find more information at https://prma-enhance.com/breast-reconstruction/diep-flap
Suzanna
Hello I am writing because I have a healing problem on my radiated left breast. I had radiation 8 years ago on the left breast, I was diagnosed again with breast cancer on my right Aug 2014.I had both breast removed, I dad my expanders removed and implants put on Oct 2015, now all of a sudden 2 months later I see my radiated side is getting a scab on it, my surgeon put me on Hyperbaric Oxygen therapy this is my first week, but today I see a little pink on the radiated side, what do you think is going to happen to me also I started antibiotic today. I also have 30 more hyperbaric sessions left. Thank you Suzana
PRMA Plastic Surgery
Hello Suzana! Without knowing your full medical history and evaluating the redness it is hard to make a clinical diagnosis. Radiation can cause complications, even after reconstruction. I would continue with the treatments your physician is recommending and then evaluate your options after.
Diane
I had a a lumpectomy and radiation in 2009. Now, a surgeon wants to do another lumpectomy for a lump he feels. I think the lump is just a side effect of radiation. Is it safe to do another lumpectomy? What tests should the doctor order first?
PRMA Plastic Surgery
Thanks so much for reaching out Diane! It is difficult to recommend a treatment plan without a full evaluation of your history with a physician. If you feel you need a second opinion before proceeding with another lumpectomy, I would recommend contacting an oncologist in your area. I hope you find this helpful.
Mai
I’m 28 turning 29 this saturday. I have my right breast removed and finished chemo. I’m now at the radiation and reconstruction stage. I don’t know what to do first. I can choose to do radiation then reconstruction using diep flap. Our I can choose implants then radiation. I’m scared and have read up on the pros and cons. I need help in deciding. I’m still young and I’m scared of the decision that I’ll be making.
PRMA Plastic Surgery
Hello Mai and thanks so much for reaching out to PRMA. Deciding between DIEP flap or implant breast reconstruction is a personal decision that should be made with the assistance of a board-certified plastic surgeon. There are pros and cons for each, but at PRMA, we typically prefer tissue flap breast reconstruction techniques (like the DIEP) anytime radiation is used for treatment.
Monica
I was recently diagnosed with stage 1 BC and I’m scheduled for a lumpectomy with lymph nodes removal later this week, and then radiation after. On top of my worrying about having a successful clear margins lumpectomy and having normal lymph nodes, I’m also worried about my silicone implants that I’ve had since July 2008. I’ve never had any complications with them but now I’m worried about possible side effects during and after my radiation treatments. I’ve read about the implant feeling hard or the implant moving higher up on your chest, shrinking, etc. What do I need to do or should I just wait and see what happens after radiation and not worry about it now? Thanks!
PRMA Plastic Surgery
Good morning Monica! I am so sorry to hear you are in this predicament! It is true that radiation and implants typically do not work well together. Usually the radiation damage causes the breast tissue and skin to change which results in dramatic differences between your breasts and usually requires additional surgery later down the road. We truly would recommend for you to seek a second opinion before proceeding. In fact, we recommend that to all of our patients if they are unsure about what to do. You are more than welcome to fill out our free virtual consultation form at or you can give our office a call at 800.692.5565. One of our board-certified surgeons would be more than happy to discuss your options with you! Hope to hear from you soon!
Tamara
Hello , in 2013 I was Dx with stage3c inflammatory breast cancer. I had all the usual, chemo, bmx with tissue expanders and radiation. I opted to do diep as advised. No true complications but I am dissatisfied with my results shape wise. So my concern from day one with the tissue expanders I had 9 months of constant pain! After diep the pain decreased about 80%. So now after 2fat grafting sessions my surgeon is recommending small silicone implants (tear drop shape I believe) above the muscle not underneath based on my experience with the TE. Surgery is scheduled for July 5th,2016. I’m caught between knowing what would be less painful in the long run vs risk of capsulation as well as the overall look. By the way it’s the projection ( or lack of that I’m displeased with) . Next is do I seek out another surgeon ( PRMA who does this all the time) or continue with my surgeon in California who has done 101 total diep with only one failure. Ultimately I know it’s my choice but would love your thoughts on this. I’m just so tired of surgeries , I’m hoping for this to be my last one!
PRMA Plastic Surgery
Hey Tamara! We would be more than happy to do a virtual consultation with you if that is something you may be interested in. This way you can get a second opinion from us before your scheduled surgery in July. You can fill out our virtual consultation form at https://prma-enhance.com/schedule-your-consultation/ and our patient liaison will connect you with one of our board-certified surgeons. I do hope we hear from you soon!
Vicky
Hi, I had a mastectomy 9 weeks ago. Expander, 240 cc fill. Doing great, full range, all looks great. Second surgery to remove expander and put in silicone implant, fat grafting from thights, lift normal breast on July 1. Radiation to start Aug. 1. What can I expect? PS knows implant may tighten and lift and plans to adjust his July 1implant placement anticipating that. Will I be ok? I do not want a third surgery! What can I do to insure success on my part?
PRMA Plastic Surgery
Hello Vicky! Unfortunately, radiation and implants typically do not go well together. We usually advise to wait until after radiation is complete before proceeding with reconstruction. If you are unsure about the plan your plastic surgeon has in place for you, I would recommend seeking a second opinion.
Vickie
I have had breast cancer and had radiation…..( on my right )….I had stage 3…… They did a lumpectomy …It was a very large mass on the top half….Now my breast are 2 different sizes… One is a little over a D and the other side is now a B…. I went to the DR… the other day to talk to him about doing something…..I’m not to sure what I want….. I was thinking about making the size D to a C and the B to a C….The DR is not to sure about doing anything to the B breast …Because I had radiation …He thinks its to much of a risk because of the radiation …I’m not sure if to take the risk or go a different rout.
PRMA Plastic Surgery
Thank you for sharing Vickie and I am so sorry to hear you are experiencing this. We would recommend seeking a second opinion to learn more about your options. We would be more than happy to consult with virtually! We offer a free virtual consultation form at https://prma-enhance.com/schedule-your-consultation/. You can also give us a call anytime at 800.692.5565
Wendy
I had breast cancer with a lumpectomy and radiation 11 years ago. I was just diagnosed with dcis in the same breast. The recommendation is to do mastectomy with tissue expanders and diep flap in a few months. Does this seem reasonable?
PRMA Plastic Surgery
Hey Wendy! It is hard to say with this minimal information what we would recommend for you. If you are unsure about your reconstruction plan, we would suggest seeking a second opinion. If you are interested, you can fill out our virtual consultation form and we would be more than happy to evaluate you case. You find the form at https://prma-enhance.com/schedule-your-consultation/
Cassandra
Hi my name is Cassandra and I was diagnosed with breast cancer at the age of 28 I had six rounds of chemo and then a double mastectomy with tissue expander placement I am now waiting to have the tissue expanders removed and permanent implants placed but this last fill that I got was very very painful, as were the ones before that. Now i have pain on right side that is radiating down my arm and back. Could this be due to a possible pinched nerve? Everyone keeps saying tissue expanders are uncomfortable but i am hurting so bad and my chest now feels like hard rock.
PRMA Plastic Surgery
Hello Cassandra! Thanks so much for reaching out to PRMA. I am so sorry to hear you are feeling so uncomfortable! Tissue expanders are typically uncomfortable. The pain and discomfort in your chest that you are experiencing should be discussed with your surgeon as soon as possible so he/she can make sure there are no complications.
Toni
I am in the same situation. I feel like someone put a rock on my chest. It’s tight and it hurts and looks awful!
PRMA Plastic Surgery
Hate to hear you are experiencing this Toni! Sadly, when radiation is involved, patients with implants can experience a lot of complications. We typically recommend removing the implants and replacing them with living healthy tissue from another area of the body. Our most commonly performed procedure is the DIEP flap. The DIEP flap uses the patient’s own abdominal skin and fat to reconstruct a natural, warm, soft breast after mastectomy. Unlike the TRAM flap, the DIEP preserves all the abdominal muscles. Only abdominal skin and fat are removed similar to a “tummy tuck”. Saving the abdominal muscles means patients experience less pain, enjoy a faster recovery, maintain their core strength long-term, and have a lower risk of complications. If you are interested, we would be more than happy to discuss your options with you further! You can reach us at 800.692.5565 or at patientadvocate@prmaplasticsurgery.com
Edgar
Sorry to hear about your situation. Hope you will get well soon. Take care.
Sabrina
Hi. In 2014 my right breast was diagnosed with stage 1 breast cancer, so I had a lumpectomy followed by 6 weeks of radiation. My right breast shrank and I experience the asymmetry. In 2016, After having a benign mass now in the left breast, my doctors performed a double mastectomy, followed by the DIEP using my stomach tissue. I am healing from the DIEP, but disappointed because my breasts are still assymetrical, with the right breast still being smaller and now darker again and hard. According to the surgeon , the size is still small because my right breast had been radiated in 2014; however, my purpose in even doing the DIEP was to bring size to the radiated breast and symmetry to both. What would be your recommendations to achieve those results now that I’ve already had the DIEP?—Disappointed Sabrina.
PRMA Plastic Surgery
Thanks for reaching our Sabrina! Typically, the DIEP flap is followed by a revision surgery to correct any symmetry issues. It is difficult to say specifically what we would recommend without consulting with you, but additional fat grafting on the smaller breast or a reduction surgery on the larger breast are both options that could help make the breast more symmetrical. We would be more than happy to review your situation and see what we could do to help. You are welcome to fill out our FREE virtual consultation form at https://prma-enhance.com/schedule-your-consultation/ and one of our surgeons would be happy to review and provide you with their recommendations. Hope this information helps!
Justina
Why is it that the expander doesn’t sail when it’s in your radiator breast that soon as you get an implant it fails what is the difference in expander and implant
PRMA Plastic Surgery
Hello Justina! Every case is different. For some, complications begin with the tissue expanders. Some patients may not experience complications until the final implant is placed, and others may never experience any complications.
Jennifer Darling
I had ductstal carsonona of right breast serger an IORT ( in operative radiation during surgery) at Hoag March 29,2017. Reconstruction and small implants were done. Thinking no other radiation was necessary. But that wade to the case. Margins were to small and I had 29 radiation treatments , July, Aug 2017. The plastic surgine results were great. Not much pain . A month after radiation pain started. October November I had a mammogram and ultrasound to see why I was having pain. Was told it was nerve pain. Everything looked fine. Dec-Jan2018 pain increased and my right breast has shrunk 50% March I had MRI, again told everything looked fine.
Why do I have pain and why is the breast shrinking. I would think the implant has failed after all that radiation. But they don’t see any problem .
Where do I go from here.
PRMA Plastic Surgery
So sorry to hear you are going through all of this Jennifer! It is difficult to say for certain what could be causing your pain and shrinkage without an evaluation, but what you describe does sound similar to common implant related complications following radiation treatments. We typically recommend replacing implants with your own living through tissue flap procedures like the DIEP flap. We welcome you to fill out our free virtual consultation form at https://prma-enhance.com/schedule-a-consultation/. Once received one of our board-certified plastic surgeons can review your needs and provide you with their surgical recommendations all from the comfort of your home.
Sending well wishes your way!
Sara
Hello, I’m going to have a bilateral mastectomy and they told me I’m going to need radiation after that. I would like to know your opinion about immediate reconstruction with adjustable implants above the muscle and if there is a difference placing the implants above or under the muscle before radiation which according to the doctor it would be 5 weeks after surgery. Thank you
PRMA Plastic Surgery
Hello Sara! Thanks so much for reaching out. We typically do not recommend implant reconstruction following radiation therapy. According to the most recent research, about 1 in 3 implant reconstructions fail following radiation treatment. It is for this reason we recommend reconstruction using your own tissue via procedures like the DIEP flap. We would be more than happy to consult with you and review your options with you. You are welcome to give us a call at 800-692-5565 or you can fill out our free virtual consultation form at https://prma-enhance.com/schedule-a-consultation/.
Christine Shields
I was not aware of the complications of a breast implant after radiation. I had implants placed in June 2018,2 capsular contractions. The first one was taken out and cleaned and put back in.After that 1st problem, I had blood pooling & 1/2 a bruised breast in lower 1/2 of my breast . Dr said it would go away. I called for a sooner appointment , I had to wait a month.That was suctioned and scraped out and a new implant was put in. That one broke through the lower 1/2 of my breast 2 large holes . It was horrible. That one was removed I am now healing very slowly. It was removed and sewn up with out any implant. That last removal was done January 29th 2019. I am at a loss of what is my next step. That breast obviously cannot handle an implant . I am reading on the DIEP. Do all Plastic Surgeons perform this? Should I risk using The same Dr again?
PRMA Plastic Surgery
So sorry to hear you are going through all of this Christine!
We are glad to hear you are researching your options! It is important to know that not all plastic surgeons perform DIEP flap reconstruction. It is important to select a surgeon who performs the procedure regularly with a high success rate. At PRMA, we perform over 700 flaps a year with an over 99% success rate. If you are ever interested in seeking a second opinion with us, we welcome you to fill out our free virtual consultation form at https://prma-enhance.com/schedule-a-consultation/
Angel Irvine
I am 3 days away from being done with radiation. This treatment is for a recurrence AFTER having diep flap with small implants. I’m starting to have some pain in breast that’s treated. Is it too soon to do a virtual consultation to have my radiated side fixed. I want implants removed and symmetry again.
Thanks for feedback.
PRMA Plastic Surgery
Thanks for reaching out Angel. You are more than welcome to fill out our free virtual consultation form at https://prma-enhance.com/schedule-a-consultation/. Once received, we can review your needs and provide you with our recommendations.
Sue Richardson
I had a double mastectomy with radiation and than expanders before the implants, biggest mistake I ever made. I have had nothing but problems with the implant on the radiated side, it has been 16 years and I’am still dealing with shrinkage and sinking on one side, I feel that it make me look like I now have a hollow dip towards the center of my chest and it makes my breast bone stick out more, I also have a lot of pain and tenderness after all these years. I have had the other side fixed so they would match in size and it didn’t last. I can live with the pain and discomfort, I have all of these years, the part I have a hard time with is moving on with your life and trying to not dwell on any future cancer when you are reminded every time you look in the mirror and every time you bump your chest and are reminded of the soreness. Almost 17 years later and I still would not recommend reconstruction on a radiated breast
PRMA Plastic Surgery
We are so sorry to hear you have had this experience Sue! We do agree with you that radiation and reconstruction with implants do not mix well. This is why we recommend reconstruction using your own tissue via “flap” options like the DIEP flap. We also want you to know, you still have options! We see women regularly who are unhappy with their implant reconstruction results and choose to have the implants removed and either “go flat” or have further reconstruction with a flap. We would be more than happy to connect with you to discuss your options and welcome you to contact us any time.