
- 0 Comments
- PRMA Plastic Surgery
July 21, 2020
What is “Flap” Breast Reconstruction?
1 in every 8 women and 1 in every 833 men are diagnosed with breast cancer. Surgical treatment options for the treatment of breast cancer include a lumpectomy or mastectomy. These can lead to very significant changes in the appearance of the breast, or even removal of the entire breast. For many patients, breast reconstruction is a good option to restore the sense of physical wholeness and confidence that was lost following the cancer surgery.
Options following a mastectomy include flat closure (ie no reconstruction), or breast reconstruction with either implants or the patient’s own tissue (known as “flap” procedures).
Flap procedures are performed either as a “pedicle” flap or a “free” flap.
A pedicle flap remains connected to the body but is moved from one area of the body (known as the “donor site”) to the breast area by being tunneled under the skin. Since the blood supply keeping this tissue alive remains connected to the body, no microsurgery is required. However, most pedicle flaps require the sacrifice of a major muscle in order to protect the blood supply keeping the “flap” alive. Most plastic surgeons are trained in pedicle flap procedures.
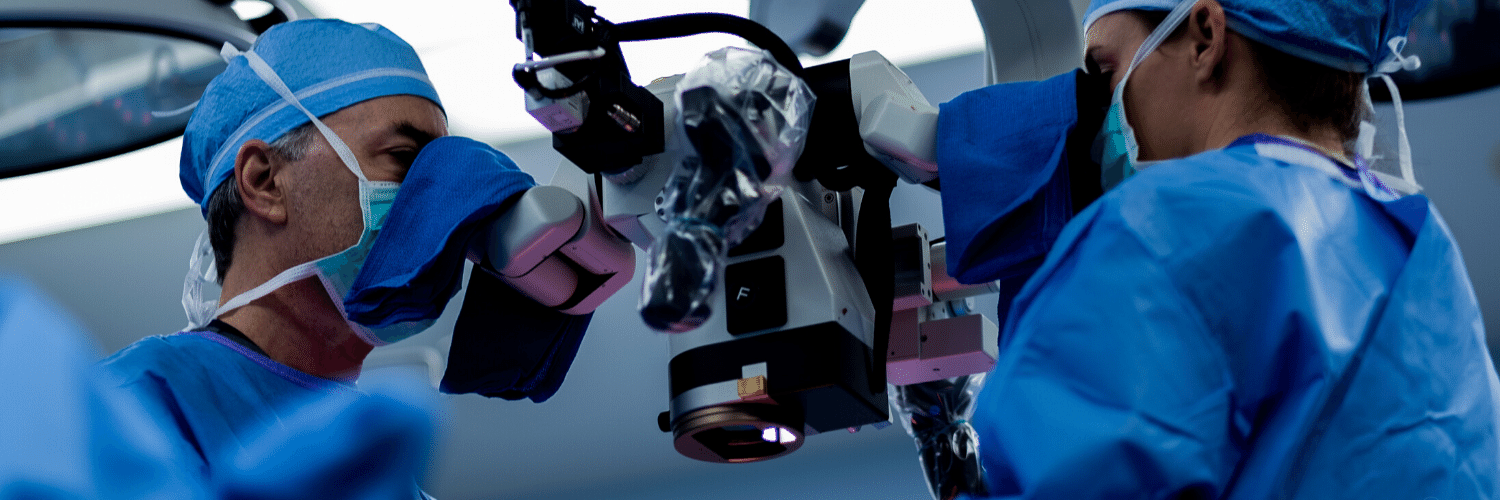
A free flap is disconnected from the body and transplanted to the breast area. This means that all connections, including the blood supply, are cut. After the tissue is transplanted to the chest, microsurgery is required in order to reconnect the artery and vein(s) needed to keep the new breast alive. Microsurgery requires specialized training and expertise. Few plastic surgeons have the necessary training and experience to offer these microsurgical procedures. Perforator flaps are the most advanced type of microsurgical reconstruction as they preserve all the patient’s muscles.
Types of Flap Procedures
Examples of pedicle flaps include:
– TRAM flap: skin, fat and one or both rectus muscle(s) (sit-up muscles) from the lower abdomen are used.
– Latissimus flap: skin, fat and the latissimus muscle from the back (shoulder blade area) are used.
Examples of perforator flaps include:
– DIEP and SIEA flaps: skin and fat from lower abdomen are used.
– Thigh flaps (eg PAP, LTP) : skin and fat from various areas of the thighs are used.
– Buttock flaps (GAP flaps): skin and fat from upper (sGAP) or lower (iGAP) buttock are used.
Regardless of the procedure being performed, more than one procedure is typically necessary for the best cosmetic results.
Pros of Flap Procedures
At PRMA, we believe perforator flap procedures are the ‘gold standard’ for breast reconstruction. Unlike implant reconstruction that creates breasts that are usually cooler to the touch and often harden over time due to build-up of scar tissue, patients who opt for flap reconstruction experience much warmer, softer and more natural results. Flap reconstruction is also permanent; it is the patient’s own living tissue, so it will never need to be replaced. Implants on the other hand often need to be replaced at least once in the patient’s lifetime.
A mastectomy usually results in complete loss of feeling in the chest area. Many perforator flaps also allow for sensory nerve reconstruction. This involves reconstructing nerves that provide feeling to the breast that were cut by the mastectomy. This additional procedure helps restore breast sensation after a mastectomy. Currently, sensory nerve reconstruction is not performed with implant reconstruction.
Cons of Flap Procedures
Because of the technical difficulty of flap-based procedures, especially perforator flaps, surgery time is typically much longer compared to implant reconstruction. To help reduce the surgery time, we use two microsurgeons for every flap surgery.
Patients opting for flap surgery will also have an additional scar from the tissue donor site.
Recovery
It is a common misconception that recovery from flap breast reconstruction is more difficult compared to implant reconstruction. However studies have shown that patients having implants placed under the chest muscle report more pain and use more narcotics than patients who have DIEP flap reconstruction.
With the implementation of our Enhanced Recovery after Surgery (ERAS) protocol, patients rarely need narcotics to control pain levels after their flap surgery. Patients begin the protocol the morning BEFORE surgery to ensure a baseline level of pain control is already in place by the time surgery begins. Our surgeons then inject very long-acting local anesthetic at the time of surgery (known as “blocks”) at each surgical site to ensure an excellent level of pain control is achieved before the patient even awakens from surgery. Most PRMA patients can maintain extremely good pain control post-operatively with non-narcotic drug combinations including Celebrex and extra-strength Tylenol.
All these improvements in recovery mean patients are up out of bed much earlier after surgery and are also ready to go home sooner; our Enhanced Recovery Protocol has decreased patient hospital stay after DIEP flap surgery to just 2-3 nights. But don’t just take our word for it! VIEW OUR PATIENT STORIES HERE.
Author: Dr. Minas Chrysopoulo and Courtney Floyd
Options following a mastectomy include flat closure (ie no reconstruction), or breast reconstruction with either implants or the patient’s own tissue (known as “flap” procedures).
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

What is “Flap” Breast Reconstruction?
PRMA Performs Record Breaking 8,500th “Natural” Breast Reconstruction Procedure
PRMA Performs Record Breaking 8,500th “Natural” Breast Reconstruction Procedure July 21, 2020 Share on Facebook Twitter Linkedin Setting a new milestone today, we have completed our 8,500th microsurgical breast reconstruction procedure. This achievement distinguishes PRMA as one of the leading breast reconstruction centers in the world. “It’s such an honor to be a part of […]

Happy 25th Anniversary PRMA Plastic Surgery
Happy 25th Anniversary PRMA Plastic Surgery July 21, 2020 Share on Facebook Twitter Linkedin The physicians and staff of PRMA Plastic Surgery celebrated the 25th anniversary of the start of the practice last week! Founded in 1994, Dr. Ledoux and Dr. Pisano began the practice with a dream to serve the San Antonio community by […]

Breast Implant Illness
Breast Implant Illness July 21, 2020 Share on Facebook Twitter Linkedin Over the years, we have seen a rise in the number of women coming to PRMA requesting to have their breast implants removed due to variety of health-related complaints, whether the implants were placed for cosmetic enhancement or for breast reconstruction following breast cancer surgery. What […]

Wearing Deodorant After Breast Reconstruction Surgery
Wearing Deodorant After Breast Reconstruction Surgery July 21, 2020 Share on Facebook Twitter Linkedin When can I resume wearing deodorant after breast reconstruction surgery? Although it may seem like a straightforward question, many patients are unsure when the appropriate time to begin applying deodorant again after surgery is. At PRMA we ask all patient to […]
The Evaluation Process for Lymphaticovenous Anastomosis
The Evaluation Process for Lymphaticovenous Anastomosis July 21, 2020 Share on Facebook Twitter Linkedin Lymphaticovenous Anastomosis (or LVA) is one of the newest surgical methods used to treat lymphedema offered at PRMA Plastic Surgery. Before a patient can undergo the procedure, extensive evaluation from a specialized reconstructive microsurgeon and a certified lymphedema therapist must take place. […]

Nipple Prosthetics Aid Reconstruction Goals for Breast Cancer Survivors
Nipple Prosthetics Aid Reconstruction Goals for Breast Cancer Survivors July 21, 2020 Share on Facebook Twitter Linkedin Some of you might say, “Nipple prosthetics…I never even knew there was such a thing.” We hear that comment quite often since we are nipple prosthetic specialists. The next sentence is usually “I wish I would have known […]

Can I Have DIEP Flap Breast Reconstruction After Prior Abdominal Surgery?
Can I Have DIEP Flap Breast Reconstruction After Prior Abdominal Surgery? July 21, 2020 Share on Facebook Twitter Linkedin Many women interested in DIEP flap breast reconstruction believe that because they have had prior abdominal surgery (such as a c-section, hysterectomy, or appendix removal) they are no longer candidates for the procedure. This is a very common […]
Causes & Correction of Abdominal Wall Weakness or Bulges after Abdominal-Based Breast Reconstruction
Causes & Correction of Abdominal Wall Weakness or Bulges after Abdominal-Based Breast Reconstruction July 21, 2020 Share on Facebook Twitter Linkedin Here is an overview of the causes of abdominal wall weakness or bulging following abdominal-based breast reconstruction and and how plastic surgeons can correct the complication. In this article you will find: 1. Benefits of using […]

Allergan Recalls Textured Implants in the U.S.
Allergan Recalls Textured Implants in the U.S. July 21, 2020 Share on Facebook Twitter Linkedin The breast implant manufacturer Allergan has officially announced it will no longer sell its Biocell textured implants or tissue expanders in the US or anywhere across the globe. The company has also asked that physicians not use any previously purchased […]

No Comments