
- 0 Comments
- PRMA Plastic Surgery
What is the impact of radiation on breast reconstruction?
Radiation therapy is often recommended as part of breast cancer treatment. Patients undergoing lumpectomy receive radiation routinely once they’ve healed from surgery. Some mastectomy patients also need radiation after surgery depending on the size and characteristics of the tumor, and lymph node status.
I think it is fair to say that most reconstructive breast surgeons are not particularly fond of radiation because of the way it can impact breast reconstruction results. Nonetheless, it is very important to remember that “life comes before breast” and in certain situations studies have shown definite benefits from radiation therapy including decreasing the risk of local recurrence and even improving overall survival.
Radiation therapy has come a long way over the years but it can still be associated with significant side effects. Radiation often causes toughening (fibrosis) and shrinking (contracture) of the patient’s tissues which makes the tissue lose its elasticity and become more firm. Skin color changes are common, red at first turning more brown over time. Radiation can also cause burn injuries (usually superficial) as well as damage to underlying organs such as the lungs and heart. Anyone who is facing radiation therapy must discuss all the potential risks with their their radiation oncologist extensively beforehand, as well discussing the potential impact on the reconstructive plan and timing with their plastic surgeon.
Radiation after a tissue (“flap”) reconstruction can cause the reconstructed breast to shrink and become firmer. Unfortunately, this is a common scenario (in varying degrees of severity) and usually exaggerates breast asymmetry. Rarely, radiation therapy can create new wounds on the reconstructed breast which need wound care. Patients facing radiation after flap breast reconstruction should know that there is a significant risk of needing further reconstructive surgery to correct changes caused by the radiation therapy and improve breast symmetry. Tissue expander / implant reconstructions usually fair much worse than flaps with radiation: the complication rates and risk of reconstructive failure in this setting are much higher than with flap reconstructions.
The timing of the reconstruction relative to the radiation therapy is also very important. While some surgeons routinely offer delayed tissue expander reconstruction to patients after mastectomy and radiation, this approach is associated with the highest risk of complications including chronic pain, poor cosmetic results, implant exposure, need for removal of the implant, and failure of the reconstruction altogether. To the contrary, delayed flap reconstruction is associated with the lowest risk of complications after radiation.
While immediate breast reconstruction with either flaps or tissue expanders can be performed in appropriate candidates when post-mastectomy radiation is planned, a coordinated team approach involving a radiation oncologist experienced in treating breast reconstruction patients is crucial in decreasing the risk of complications.
Author: Dr. Minas Chrysopoulo
Anyone who is facing radiation therapy must discuss all the potential risks with their their radiation oncologist extensively beforehand, as well discussing the potential impact on the reconstructive plan and timing with their plastic surgeon.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

What is the impact of radiation on breast reconstruction?

Holiday Stress and Breast Cancer
Holiday Stress and Breast Cancer July 08, 2020 Share on Facebook Twitter Linkedin How can you reduce stress around the holidays? Holiday stress is hard to avoid and when you add breast cancer to the hype of the holidays, you may feel especially overwhelmed. We recently had the opportunity to invite Sylvia Villareal, a certified […]
Achieving Breast Symmetry in the Delayed vs Immediate Breast Reconstruction Patient
Achieving Breast Symmetry in the Delayed vs Immediate Breast Reconstruction Patient July 08, 2020 Share on Facebook Twitter Linkedin How do surgeons create symmetry during delayed breast reconstruction? In my last blog we discussed the topic of breast reconstruction in the setting of prophylactic mastectomy for breast cancer prevention for women carrying one of the […]

Best Places to Work: PRMA Plastic Surgery
Best Places to Work: PRMA Plastic Surgery July 08, 2020 Share on Facebook Twitter Linkedin The other day I did a search for the best jobs in America and found that working in the healthcare industry is by far one of the best fields to be in. Going to school for PR and marketing I […]
BRCA Gene Mutation, Prophylactic Mastectomy & Breast Reconstruction
BRCA Gene Mutation, Prophylactic Mastectomy & Breast Reconstruction July 08, 2020 Share on Facebook Twitter Linkedin What are your options to reduce your risk of hereditary breast cancer? Earlier this week celebrity Sharon Osbourne announced that she was having bilateral (double) mastectomies to prevent cancer because there is a hereditary pattern of breast cancer in […]
Surgical Drains After Breast Reconstruction – What To Expect
Surgical Drains After Breast Reconstruction – What To Expect July 08, 2020 Share on Facebook Twitter Linkedin What should you expect with surgical drains after breast reconstruction? If you are contemplating breast reconstruction or are already scheduled for surgery, chances are you have questions about the surgical drains that follow. The drains, called Jackson-Pratt or […]
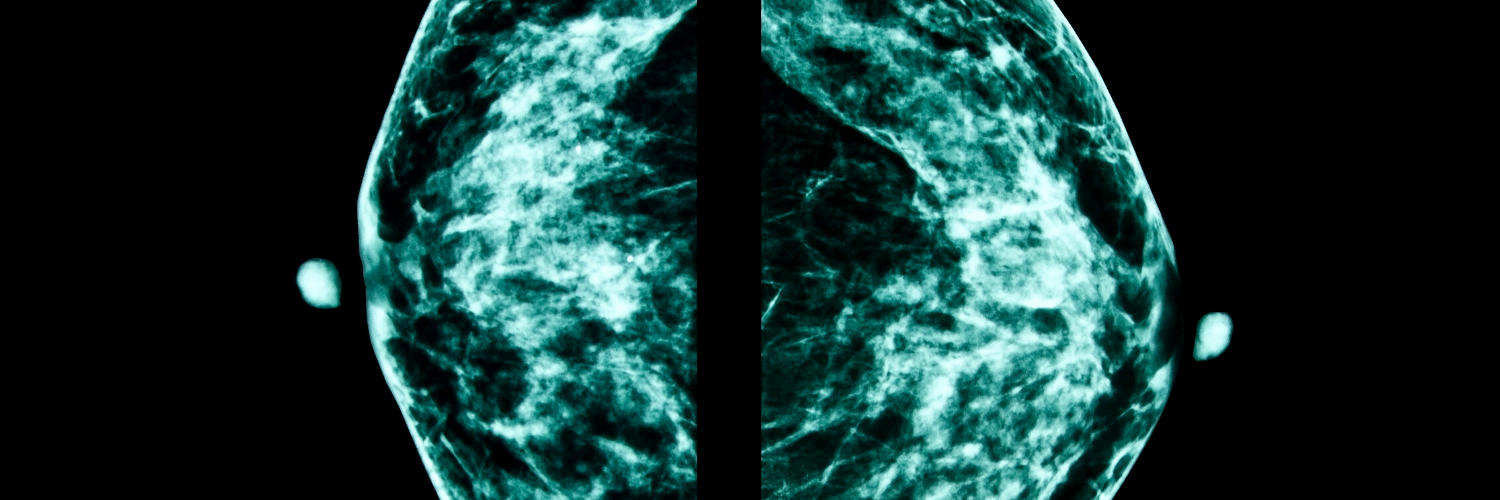
Breast Density and Risk of Breast Cancer – What’s the Scoop?
Breast Density and Risk of Breast Cancer – What’s the Scoop? July 08, 2020 Share on Facebook Twitter Linkedin Does breast density impact your breast cancer risk? There has been a lot of talk recently about breast density and how it affects breast cancer screening. After California, Texas and several other states enacted new legislation […]
Research Performed at PRMA Proves Safety of DIEP Flap Reconstruction in Obese Patients
PRMA Proves Safety of DIEP Flap Reconstruction in Obese Patients July 08, 2020 Share on Facebook Twitter Linkedin Is DIEP flap breast reconstruction safe for obese patients? As more women choose the DIEP flap for breast reconstruction after mastectomy, some patients are unnecessarily turned away because they are overweight. Surgeons at PRMA Plastic Surgery say […]

Immediate Breast Reconstruction Plays Significant Role in Physical and Psychological Wellbeing
Immediate Breast Reconstruction Plays Significant Role in Physical and Psychological Wellbeing July 08, 2020 Share on Facebook Twitter Linkedin Does immediate breast reconstruction help breast cancer patients heal psychologically? Immediate breast reconstruction after mastectomy has significant benefits on the psychological and social well being of breast cancer survivors, according to a study done by Toronto […]

Tattoos Not Just For Fashion
Tattoos Not Just For Fashion July 08, 2020 Share on Facebook Twitter Linkedin How are tattoos used to help breast cancer patients? San Antonio, TX–Tattoos have been used for centuries for fashion and decoration, but today tattooing is also helping breast cancer patients feel whole again. After her breast reconstruction surgery last year, 33 year […]


No Comments