
- 0 Comments
- PRMA Plastic Surgery
When Should You Consider Prophylactic Mastectomy of The Non-Cancer Breast?
Having breast cancer in one breast increases a woman’s chances of getting breast cancer in the second breast at some point. Unless the patient is “high risk” (eg BRCA+), this risk peaks at about 20% over the patient’s lifetime in women diagnosed with their first cancer at a young age.
While contralateral prophylactic mastectomy (ie removing the healthy opposite breast as well as the breast with cancer) decreases the risk of future breast cancer in the opposite breast, several studies have shown that this does not improve long term survival. A study in the journal Cancer tries to address a question which women facing mastectomy for breast cancer have been asking doctors for years… should I have my healthy breast removed as well to decrease my risk of another breast cancer?
Here’s the study abstract:
Predictors of contralateral breast cancer in patients with unilateral breast cancer undergoing contralateral prophylactic mastectomy. Min Yi, Funda Meric-Bernstam, Lavinia P. Middleton, et al. CANCER Print Issue Date: March 1, 2009
BACKGROUND:
Although contralateral prophylactic mastectomy (CPM) reduced the risk of contralateral breast cancer in unilateral breast cancer patients, it was diffcult to predict which patients were most likely to benefit from the procedure. The objective of this study was to identify the clinicopathologic factors that predict contralateral breast cancer and thereby inform decisions regarding performing CPM in unilateral breast cancer patients.
METHODS:
A total of 542 unilateral breast cancer patients who underwent CPM at The University of Texas M. D. Anderson Cancer Center from January 2000 to April 2007 were included in the current study. A logistic regression analysis was used to identify clinicopathologic factors that predict contralateral breast cancer.
RESULTS:
Of the 542 patients included in this study, 25 (5 %) had an occult malignancy in the contralateral breast. Eighty-two patients (15 %) had moderate-risk to high-risk histologic findings identified at final pathologic evaluation of the contralateral breast. Multivariate analysis revealed that 3 independent factors predicted malignancy in the contralateral breast: an ipsilateral invasive lobular histology, an ipsilateral multicentric tumor, and a 5-year Gail risk 1.67 %. Multivariate analysis also revealed that an age of 50 years at the time of the initial cancer diagnosis and an additional ipsilateral moderate-risk to high-risk pathology were independent predictors of moderate-risk to high-risk histologic findings in the contralateral breast.
CONCLUSIONS:
The findings indicated that CPM may be a rational choice for breast cancer patients who have a 5-year Gail risk 1.67 %, an additional ipsilateral moderate-risk to high-risk pathology, an ipsilateral multicentric tumor, or an ipsilateral tumor of invasive lobular histology.
So what does this mean?
In breast cancer patients choosing mastectomy, we already know that it is very appropriate for those who are “high risk” to consider mastectomy of the healthy breast too (contralateral prophylactic mastectomy). By “high risk” we mean patients with a genetic predisposition to breast cancer (eg mutations in BRCA, TP53, PALB, etc) and those with strong family histories. This study suggests that the following factors should also be taken in to account when considering contralateral prophylactic mastectomy:
1) the patient has a breast cancer that is particularly aggressive or invasive
2) the biopsy pathology report shows high risk histology (such as “invasive lobular” disease)
3) there are multiple tumors in the same breast
4) the patient’s 5-year Gail risk is at least 1.67 – The “Gail risk” assesses a woman’s risk of developing breast cancer by looking at a number of health factors including her medical history, race, age and more. Your medical oncologist will be able to tell you your Gail score.
5) the patient is 50yrs old or younger at the time of the first breast cancer diagnosis.
This study does not address the impact of other factors that invariably come into play like breast symmetry, anxiety over frequent screening tests, fear of future disease and other quality of life issues. Ultimately, the decision is a very personal one and these factors also need to be considered.
Author: Dr. Minas Chrysopoulo
Having breast cancer in one breast increases a woman’s chances of getting breast cancer in the second breast at some point. Unless the patient is “high risk” (eg BRCA+), this risk peaks at about 20% over the patient’s lifetime in women diagnosed with their first cancer at a young age.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

When Should You Consider Prophylactic Mastectomy of The Non-Cancer Breast?

Leslie Mouton’s Breast Reconstruction Diary
Leslie Mouton’s Breast Reconstruction Diary July 07, 2020 Share on Facebook Twitter Linkedin What’s it like to have breast reconstruction? PRMA Plastic Surgery would like to thank Mrs. Leslie Mouton, local news anchor for KSAT12 News in San Antonio, for documenting her experiences with breast cancer reconstruction. We hope that patients are able to gain […]

Cosmetic Surgery-Breast Procedures
Cosmetic Surgery-Breast Procedures July 07, 2020 Share on Facebook Twitter Linkedin What are the different cosmetic surgery options offered at PRMA Plastic Surgery? Our experienced surgeons offer breast augmentation (enhancement) with breast implants, breast lift (mastopexy), and breast reduction procedures. These procedures help create an aesthetically pleasing look for women who are self-conscious about their […]
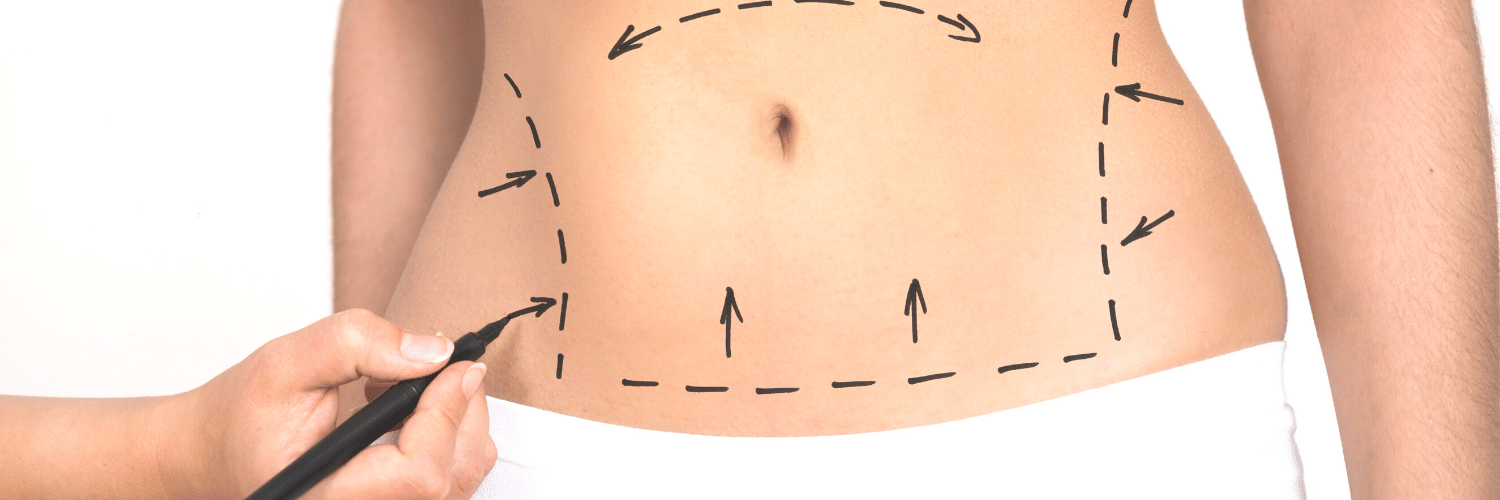
Liposuction, Tummy Tuck (Abdominoplasty) & Body Lift
Liposuction, Tummy Tuck (Abdominoplasty) & Body Lift July 07, 2020 Share on Facebook Twitter Linkedin What are cosmetic surgery options to improved body contour? Patients seeking an improvement in body contour are usually candidates for either liposuction, a tummy tuck (abdominoplasty), a body lift, or some combination of these procedures. Our experienced plastic surgeons help […]
Microsurgical Breast Reconstruction With Perforator Flaps
Microsurgical Breast Reconstruction With Perforator Flaps July 07, 2020 Share on Facebook Twitter Linkedin What are perforator flaps? How are they used in breast reconstruction? Microsurgical breast reconstruction using perforator flaps represents the state of the art in reconstructive breast surgery after mastectomy. The tissue removed by the mastectomy is replaced with the patient’s own […]
Reconstructive Breast Surgery – Part III – Perforator Flaps
Reconstructive Breast Surgery – Part III – Perforator Flaps July 07, 2020 Share on Facebook Twitter Linkedin What are the breast reconstruction options using your own tissue? The ideal breast reconstruction technique is one which allows reconstruction of a “natural”, warm, soft breast with the least impact on the patient’s body. While breast reconstruction with […]

Reconstructive Breast Surgery – Part II – Muscle Flaps
Reconstructive Breast Surgery – Part II – Muscle Flaps July 07, 2020 Share on Facebook Twitter Linkedin What breast reconstruction options use muscle? Women interested in breast reconstruction after mastectomy have several reconstruction options to choose from. In Part I of this series we discussed tissue expanders, breast implants and Alloderm. Though implant reconstruction remains […]

Reconstructive Breast Surgery – Part I – Tissue Expanders, Breast Implants and Alloderm
Reconstructive Breast Surgery – Part I – Tissue Expanders, Breast Implants and Alloderm July 07, 2020 Share on Facebook Twitter Linkedin What breast reconstruction options use implants? This post is the first of a 3-part series on reconstructive breast surgery discussing the reconstructive options available to women facing mastectomy for breast cancer. Every woman has […]
Breast Reconstruction With Tissue Much Safer Than Implants When Radiation Planned After Mastectomy
Breast Reconstruction With Tissue Much Safer Than Implants When Radiation Planned After Mastectomy July 07, 2020 Share on Facebook Twitter Linkedin Is breast reconstruction using your own tissue safe? A study published in the November issue of the International Journal of Radiation Oncology-Biology-Physics examined the effect of radiation therapy on different methods of immediate breast […]

Breast Cancer Recurrence Not Influenced By Method Of Breast Reconstruction
Breast Cancer Recurrence Not Influenced By Method Of Breast Reconstruction July 07, 2020 Share on Facebook Twitter Linkedin Does breast reconstruction increase the chance of breast cancer recurrence? One of my out-of-state breast cancer patients called me today. She recently underwent bilateral mastectomies and immediate breast reconstruction with DIEP flaps. She recovered very well from […]


No Comments