- 1 Comment
- PRMA Plastic Surgery
How do surgeons create symmetry during delayed breast reconstruction?
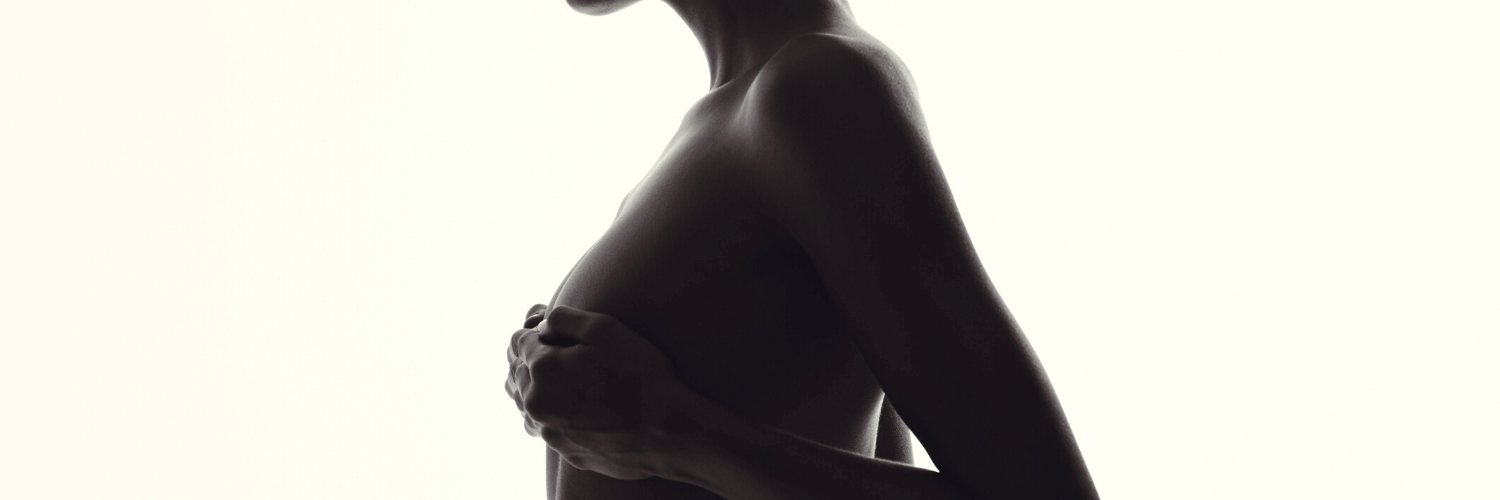
In my last blog we discussed the topic of breast reconstruction in the setting of prophylactic mastectomy for breast cancer prevention for women carrying one of the BRCA gene mutations. In this circumstance it is generally relatively easy to achieve symmetry of size and shape of the reconstructed breasts (notice I qualified this statement with the word relatively) . We, or the general surgeon performing the mastectomies, can leave the skin envelope of the breast thicker; we can stay within the footprint of the breast, especially respecting the inframammary fold; nipple-areola sparing mastectomies can be performed. All of these factors contribute to symmetry of size and shape.
In contrast to the above scenario, the surgeons of PRMA are frequently confronted with the breast cancer patient who requires a prophylactic mastectomy on one side (again, the relatively easy reconstructive situation) and a delayed reconstruction on the other. Here the mastectomy has already been done on the cancer side. Often the mastectomy has been “aggressive”, meaning a significant portion of the breast skin envelope has been removed and the overall footprint of the breast – including the inframammary fold, lateral (outer) breast-chest wall border, and superior (upper) breast-chest wall boundary – has been destroyed. In many cases the mastectomy has been followed by radiation therapy. Radiation makes the remaining skin envelope tight, firm, dry, hyperprigmented (reddish-brown to dark brown), and tethered to the chest wall. The mastectomy-radiation defect is by definition a severe defect; reconstructions in this setting are challenging.
Achieving symmetry of size and shape is difficult in the delayed vs immediate reconstruction patient. These patients are generally poor expander-implant candidates, at least on the delayed reconstruction side which has usually been radiated; these patients usually receive an autologous tissue reconstruction, most commonly with the DIEP flap. We almost never perform an implant reconstruction in the setting of chest wall radiation. The delayed side requires more skin replacement (often some of the irradiated skin must be excised, making the skin requirement even greater) and more volume. The boundaries of the breast must be restored. Because radiation makes the native breast and chest wall skin tight and tethered it is difficult to achieve the proper amount of projection – that is, the height of the breast off the chest wall in profile view – compared to the immediately reconstructed breast, which has the soft, elastic native breast skin.
The surgeons of PRMA employ a variety of strategies in an effort to overcome the challenges of the delayed vs immediate breast reconstruction patient. We make the flap for the delayed side larger and include more skin from the abdomen; we attempt to restore the proper boundaries of the breast; the flap to the immediate side may be smaller. Then, at the second stage operation, we will add volume to the delayed side in the form of autologous fat graft; fat grafting can also help us restore the transition area between the chest wall and breast in the upper and inner areas.
These strategies usually enable us to achieve reasonably good symmetry between the delayed and immediate sides; however, it is important to recognize that in most patients some asymmetry will persist, and in some patients, albeit a relative minority, the asymmetry will be quite pronounced. A high degree of satisfaction is very difficult to achieve in this last group. In my 18 years of experience involving literally thousands of flap reconstruction procedures I have found that this subset of reconstruction patients is usually less pleased with the reconstruction outcome than the bilateral (double) immediate or bilateral delayed patient.
Additional fat grafting to the delayed side and/or placement of an implant under the DIEP flap may be possible and may help (of note, in our experience at PRMA we have found that the major insurance carriers for this geographic area will not cover these adjunctive procedures; alternatively, carriers may cover them for other practices in different, neighboring practices).
The key to reaching a satisfactory outcome in the delayed vs immediate breast reconstruction patient is for the surgeon to set – and for the patient to understand and accept – reasonable expectations. We will likely not achieve perfect symmetry of size and shape, but we likely will end up with an attractive reconstructed breast on the delayed side. With this expectation met, we can restore a sense of wholeness to the patient.
Author: Dr. Steven Pisano
The key to reaching a satisfactory outcome in the delayed vs immediate breast reconstruction patient is for the surgeon to set – and for the patient to understand and accept – reasonable expectations. We will likely not achieve perfect symmetry of size and shape, but we likely will end up with an attractive reconstructed breast on the delayed side. With this expectation met, we can restore a sense of wholeness to the patient.
Leave Comment
No Comments
Sign Up for Our Monthly Newsletter
Continue Reading
Achieving Breast Symmetry in the Delayed vs Immediate Breast Reconstruction Patient

Best Places to Work: PRMA Plastic Surgery
Best Places to Work: PRMA Plastic Surgery July 08, 2020 Share on Facebook Twitter Linkedin The other day I did a search for the best jobs in America and found that working in the healthcare industry is by far one of the best fields to be in. Going to school for PR and marketing I […]
BRCA Gene Mutation, Prophylactic Mastectomy & Breast Reconstruction
BRCA Gene Mutation, Prophylactic Mastectomy & Breast Reconstruction July 08, 2020 Share on Facebook Twitter Linkedin What are your options to reduce your risk of hereditary breast cancer? Earlier this week celebrity Sharon Osbourne announced that she was having bilateral (double) mastectomies to prevent cancer because there is a hereditary pattern of breast cancer in […]
Surgical Drains After Breast Reconstruction – What To Expect
Surgical Drains After Breast Reconstruction – What To Expect July 08, 2020 Share on Facebook Twitter Linkedin What should you expect with surgical drains after breast reconstruction? If you are contemplating breast reconstruction or are already scheduled for surgery, chances are you have questions about the surgical drains that follow. The drains, called Jackson-Pratt or […]
Breast Density and Risk of Breast Cancer – What’s the Scoop?
Breast Density and Risk of Breast Cancer – What’s the Scoop? July 08, 2020 Share on Facebook Twitter Linkedin Does breast density impact your breast cancer risk? There has been a lot of talk recently about breast density and how it affects breast cancer screening. After California, Texas and several other states enacted new legislation […]
Research Performed at PRMA Proves Safety of DIEP Flap Reconstruction in Obese Patients
PRMA Proves Safety of DIEP Flap Reconstruction in Obese Patients July 08, 2020 Share on Facebook Twitter Linkedin Is DIEP flap breast reconstruction safe for obese patients? As more women choose the DIEP flap for breast reconstruction after mastectomy, some patients are unnecessarily turned away because they are overweight. Surgeons at PRMA Plastic Surgery say […]

Immediate Breast Reconstruction Plays Significant Role in Physical and Psychological Wellbeing
Immediate Breast Reconstruction Plays Significant Role in Physical and Psychological Wellbeing July 08, 2020 Share on Facebook Twitter Linkedin Does immediate breast reconstruction help breast cancer patients heal psychologically? Immediate breast reconstruction after mastectomy has significant benefits on the psychological and social well being of breast cancer survivors, according to a study done by Toronto […]

Tattoos Not Just For Fashion
Tattoos Not Just For Fashion July 08, 2020 Share on Facebook Twitter Linkedin How are tattoos used to help breast cancer patients? San Antonio, TX–Tattoos have been used for centuries for fashion and decoration, but today tattooing is also helping breast cancer patients feel whole again. After her breast reconstruction surgery last year, 33 year […]

Several Options available for Breast Reconstruction with Implants
Several Options available for Breast Reconstruction with Implants July 08, 2020 Share on Facebook Twitter Linkedin What are the different implant breast reconstruction options? Every year one in eight women will be diagnosed with breast cancer. Many are opting for the DIEP flap procedure as a reconstruction option after mastectomy, but some may not be candidates. For […]
Reconstructing Breasts with Feeling
Reconstructing Breasts with Feeling July 08, 2020 Share on Facebook Twitter Linkedin Do you still have breast feeling after a mastectomy and breast reconstruction? Most women facing mastectomy and breast reconstruction want to know what kind of feeling their new breast(s) will have. Unfortunately mastectomy leaves many women with very little feeling long term (if […]


Anonymous
Detailed and straightforward explanations, Dr. Pisano, are part of PRMA’s practice that lead to informed patients. Great blog with valuable information. Thanks much!