- 2 Comments
- PRMA Plastic Surgery
What are your options to reduce your risk of hereditary breast cancer?
Earlier this week celebrity Sharon Osbourne announced that she was having bilateral (double) mastectomies to prevent cancer because there is a hereditary pattern of breast cancer in her family. This announcement brings the concept of hereditary forms of breast cancer into the public domain, and offers an opportunity to educate men and women about genetic testing and treatment options.
Specifically, BRCA1 and BRCA2 are human genes that are part of a class of genes known as tumor suppressors. A harmful mutation of either of these genes confers a markedly increased chance of developing breast and/or ovarian cancer over a woman’s lifetime (of note, men also carry the BRCA genes, and a harmful mutation in one of them increases the risk of breast, prostate, and possibly other cancers). It is estimated that about 12% of women in the general population will develop breast cancer at some point in their lives; among women with a BRCA1 or BRCA2 mutation 60% will develop breast cancer. It is important to appreciate that most women who develop breast cancer do not carry a BRCA mutation. In the majority of cases breast cancer is said to be “sporadic”. Breast (and/or ovarian) cancer is most likely associated with a BRCA mutation in families with a history of multiple cases of breast cancer, combinations of breast and ovarian cancer, or cases in which a family member has had more than one type of cancer. Women with these family history cancer patterns should consider genetic counseling and possibly genetic testing.
For the woman who carries a BRCA mutation there are a number of options, including: surveillance, prophylactic surgery, and risk reduction with certain medications. The core service at PRMA is breast reconstruction. An increasing number of women who undergo reconstruction with us are women with a BRCA1 or BRCA2 mutation. The surgical approach involves bilateral mastectomies – with or without sparing the nipple-areola tissue – followed by immediate reconstruction. The goal of the mastectomies is to remove as much of the at risk breast tissue as possible without compromising the short and long term quality of the native breast skin; removing absolutely all breast tissue is difficult if not impossible, and therefore, mastectomies are not a guarantee that a BRCA carrier will not develop breast cancer.
For women who elect to have mastectomies implant-based or tissue-based breast reconstruction is available. Implant reconstruction can be either a single stage or two stage procedure; in the two stage method a short-term tissue expander is placed before the final implant. Implant reconstruction can also be accompanied by placement of additional material called acellular dermal matrix, a protein substance that provides additional coverage over the implant besides the native breast skin. There are many tissue-based (autologous) breast reconstruction options. In our practice at PRMA the DIEP flap is the most commonly chosen method of autologous tissue breast reconstruction – and the most commonly performed method of breast reconstruction overall.
With a well-executed mastectomy and reconstruction – especially an autologous reconstruction – the BRCA patient can have a very positive outcome, in which breast cancer risk is greatly reduced, and the size, shape and consistency of the breasts approaches normal.
Author: Dr. Steven Pisano
For the woman who carries a BRCA mutation there are a number of options, including: surveillance, prophylactic surgery, and risk reduction with certain medications
Leave Comment
No Comments
Sign Up for Our Monthly Newsletter
Continue Reading
BRCA Gene Mutation, Prophylactic Mastectomy & Breast Reconstruction
Surgical Drains After Breast Reconstruction – What To Expect
Surgical Drains After Breast Reconstruction – What To Expect July 08, 2020 Share on Facebook Twitter Linkedin What should you expect with surgical drains after breast reconstruction? If you are contemplating breast reconstruction or are already scheduled for surgery, chances are you have questions about the surgical drains that follow. The drains, called Jackson-Pratt or […]
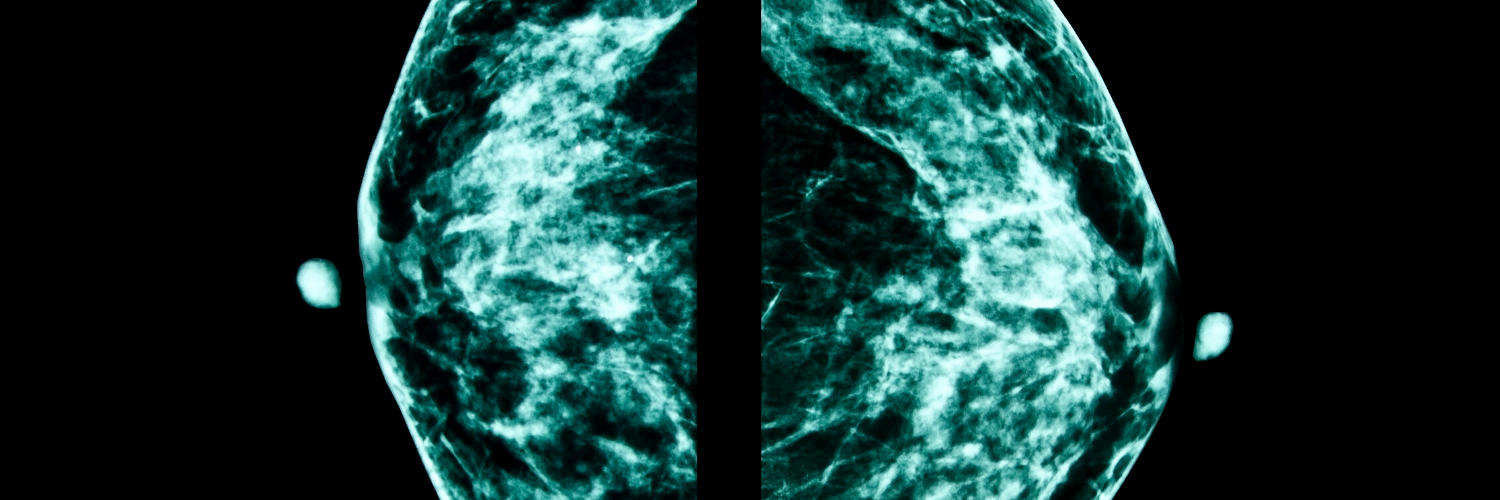
Breast Density and Risk of Breast Cancer – What’s the Scoop?
Breast Density and Risk of Breast Cancer – What’s the Scoop? July 08, 2020 Share on Facebook Twitter Linkedin Does breast density impact your breast cancer risk? There has been a lot of talk recently about breast density and how it affects breast cancer screening. After California, Texas and several other states enacted new legislation […]
Research Performed at PRMA Proves Safety of DIEP Flap Reconstruction in Obese Patients
PRMA Proves Safety of DIEP Flap Reconstruction in Obese Patients July 08, 2020 Share on Facebook Twitter Linkedin Is DIEP flap breast reconstruction safe for obese patients? As more women choose the DIEP flap for breast reconstruction after mastectomy, some patients are unnecessarily turned away because they are overweight. Surgeons at PRMA Plastic Surgery say […]

Immediate Breast Reconstruction Plays Significant Role in Physical and Psychological Wellbeing
Immediate Breast Reconstruction Plays Significant Role in Physical and Psychological Wellbeing July 08, 2020 Share on Facebook Twitter Linkedin Does immediate breast reconstruction help breast cancer patients heal psychologically? Immediate breast reconstruction after mastectomy has significant benefits on the psychological and social well being of breast cancer survivors, according to a study done by Toronto […]

Tattoos Not Just For Fashion
Tattoos Not Just For Fashion July 08, 2020 Share on Facebook Twitter Linkedin How are tattoos used to help breast cancer patients? San Antonio, TX–Tattoos have been used for centuries for fashion and decoration, but today tattooing is also helping breast cancer patients feel whole again. After her breast reconstruction surgery last year, 33 year […]

Several Options available for Breast Reconstruction with Implants
Several Options available for Breast Reconstruction with Implants July 08, 2020 Share on Facebook Twitter Linkedin What are the different implant breast reconstruction options? Every year one in eight women will be diagnosed with breast cancer. Many are opting for the DIEP flap procedure as a reconstruction option after mastectomy, but some may not be candidates. For […]
Reconstructing Breasts with Feeling
Reconstructing Breasts with Feeling July 08, 2020 Share on Facebook Twitter Linkedin Do you still have breast feeling after a mastectomy and breast reconstruction? Most women facing mastectomy and breast reconstruction want to know what kind of feeling their new breast(s) will have. Unfortunately mastectomy leaves many women with very little feeling long term (if […]

Fat Grafting in Breast Reconstruction – What You Need To Know
Fat Grafting in Breast Reconstruction – What You Need To Know July 08, 2020 Share on Facebook Twitter Linkedin What is fat grafting? How is fat grafting used in breast reconstruction? Fat grafting, as a technique, has been around for many years but has recently experienced a resurgence in breast surgery. The procedure involves liposuctioning […]

What is Alloderm Breast Reconstruction?
What is Alloderm Breast Reconstruction? July 08, 2020 Share on Facebook Twitter Linkedin What is Alloderm? Alloderm, and other similar ADM products including Strattice and FlexHD, are now being used routinely in breast reconstruction. ADM stands for “acellular dermal matrix”. It is a biologic mesh-like material derived from animals or donated (cadaveric) human skin. Alloderm is a human […]

Surgical Drains After Breast Reconstruction – What To Expect
Best Places to Work: PRMA Plastic Surgery

Holly
I have been diagnosed with a radial scar and have a positive PALB2 gene mutation. I have 2 sisters that have been diagnosed with breast cancer. The first sister was a triple negative and received the TRAM with the DIEP Flap reconstruction with PRMA. She was diagnosed at 48 (it’s been 10 years). The second sister was diagnosed at age 52. She tested positive to the 2 hormone receptors estrogen and progesterone. Based on my family history and genetic test results it has been recommend that I have prophylactic mastectomies. I would like to schedule an appointment to hear about my options. Do I need a referral from my PCP? What are the necessary steps to start the process? I live in San Angelo, Texas.
PRMA Plastic Surgery
Hello Holly! Thanks for reaching out to PRMA! We would be more than happy to set you up a consult to discuss your options for prophylactic surgery. Please give our office a call at 210-692-1181 and one of our office staff can find a time that works best for you.