
- 0 Comments
- PRMA Plastic Surgery
Can breast cancer be detected early?
Breast Cancer Screening Recommendations from the American Cancer Society
Screening refers to tests and exams used to find a disease, such as cancer, in people who do not have any symptoms. The goal of screening exams, such as mammograms, is to find cancers before they start to cause symptoms. Breast cancers that are found because they can be felt tend to be larger and are more likely to have already spread beyond the breast. In contrast, breast cancers found during screening exams are more likely to be small and still concerned to the breast. The size of a breast cancer and how far it has spread are important factors in predicting the prognosis (survival outlook) for a woman with this disease.
Most doctors feel that early detection tests for breast cancer save many thousands of lives each year, and that many more lives could be saved if even more women and their health care providers took advantage of these tests. Following the American Cancer Society’s guidelines for the early detection of breast cancer improves the chances that breast cancer can be diagnosed at an early stage and treated successfully.
American Cancer Society recommendations for early breast cancer detection. Women age 40 and older should have a screening mammogram every year and should continue to do so for as long as they are in good health.
Current evidence supporting mammograms is even stronger than in the past. In particular, recent evidence has confirmed that mammograms offer substantial benefit for women in their 40s. Women can feel confident about the benefits associated with regular mammograms for finding cancer early.
However, mammograms also have limitations. A mammogram will miss some cancers, and it sometimes leads to follow up of findings that are not cancer, including biopsies.
Women should be told about the benefits, limitations, and potential harms linked with regular screening. Mammograms can miss some cancers. But despite their limitations, they remain a very effective and valuable tool for decreasing suffering and death from breast cancer.
Mammograms for older women should be based on the individual, her health, and other serious illnesses, such as congestive heart failure, end-stage renal disease, chronic obstructive pulmonary disease, and moderate-to-severe dementia. Age alone should not be the reason to stop having regular mammograms.
As long as a woman is in good health and would be a candidate for treatment, she should continue to be screened with a mammogram.
Women in their 20s and 30s should have a clinical breast exam (CBE) as part of a periodic (regular) health exam by a health professional, at least every 3 years. After age 40, women should have a breast exam by a health professional every year. CBE is a complement to mammograms and an opportunity for women and their doctor or nurse to discuss changes in their breasts, early detection testing, and factors in the woman’s history that might
make her more likely to have breast cancer.
There may be some benefit in having the CBE shortly before the mammogram. The exam should include instruction for the purpose of getting more familiar with your own breasts. Women should also be given information about the benefits and limitations of CBE and breast self exam (BSE). Breast cancer risk is very low for women in their 20s and gradually increases with age. Women should be told to promptly report any new breast symptoms to a health professional.
Breast self exam (BSE) is an option for women starting in their 20s. Women should be told about the benefits and limitations of BSE. Women should report any breast changes to their health professional right away. Research has shown that BSE plays a small role in finding breast cancer compared with finding a breast lump by chance or simply being aware of what is normal for each woman. Some women feel very comfortable doing BSE regularly (usually monthly after their period) which involves a systematic step-by-step approach to examining the look and feel of their breasts.
Other women are more comfortable simply looking and feeling their breasts in a less systematic approach, such as while showering or getting dressed or doing an occasional thorough exam. Sometimes, women are so concerned about “doing it right” that they become stressed over the technique. Doing BSE regularly is one way for women to know how their breasts normally look and feel and to notice any changes. The goal, with or without BSE, is to report any breast changes to a doctor or nurse right away.
Women who choose to do BSE should have their BSE technique reviewed during their physical exam by a health professional. It is okay for women to choose not to do BSE or not to do it on a regular schedule. However, by doing the exam regularly, you get to know how your breasts normally look and feel and you can more readily detect any signs or symptoms if a change occurs, such as development of a lump or swelling, skin irritation or dimpling, nipple pain or retraction (turning inward), redness or scaliness of the nipple or breast skin, or a discharge other than breast milk.
Should you notice any changes you should see your health care provider as soon as possible for evaluation. Remember that most of the time, however, these breast changes are not cancer. Women at high risk (greater than 20 % lifetime risk) should get an MRI and a mammogram every year.
Women at moderately increased risk (15 % to 20 % lifetime risk) should talk with their doctors about the benefits and limitations of adding MRI screening to their yearly mammogram. Yearly MRI screening is not recommended for women whose lifetime risk of breast cancer is less than 15 %.
Women at high risk include those who:
have a known BRCA1 or BRCA2 gene mutation
have a first-degree relative (parent, brother, sister, or child) with a BRCA1 or BRCA2 gene mutation, but have not had genetic testing themselves
have a lifetime risk of breast cancer of 20 % to 25 % or greater, according to risk assessment tools that are based mainly on family history (see below)
had radiation therapy to the chest when they were between the ages of 10 and 30 years
have Li-Fraumeni syndrome, Cowden syndrome, or Bannayan-Riley-Ruvalcaba syndrome, or have first-degree relatives with one of these syndromes
Women at moderately increased risk include those who:
have a lifetime risk of breast cancer of 15 % to 20 %, according to risk assessment tools that are based mainly on family history (see below)
have a personal history of breast cancer, ductal carcinoma in situ (DCIS), lobular carcinoma in situ (LCIS), atypical ductal hyperplasia (ADH), or atypical lobular hyperplasia (ALH)
have extremely dense breasts or unevenly dense breasts when viewed by mammograms.
If MRI is used, it should be in addition to, not instead of, a screening mammogram. This is because while an MRI is a more sensitive test (it’s more likely to detect cancer than a mammogram), it may still miss some cancers that a mammogram would detect. For most women at high risk, screening with MRI and mammograms should begin at age 30 years and continue for as long as a woman is in good health. But because the evidence is limited regarding the best age at which to start screening, this decision should be based on shared decision making between patients and their health care providers, taking into account personal circumstances and preferences.
Several risk assessment tools, with names such as the Gail model, the Claus model, and the Tyrer-Cuzick model, are available to help health professionals estimate a woman’s breast cancer risk. These tools give approximate, rather than precise, estimates of breast cancer risk based on different combinations of risk factors and different data sets. As a result, they may give different risk estimates for the same woman. Their results should be discussed by a woman and her doctor when being used to decide whether to start MRI screening.
It is recommended that women who get screening MRI do so at a facility that can do an MRI-guided breast biopsy at the same time if needed. Otherwise, the woman will have to have a second MRI exam at another facility at the time of biopsy. There is no evidence right now that MRI will be an effective screening tool for women at average risk. While MRI is more sensitive than mammograms, it also has a higher false-positive rate (it is more likely to find something that turns out not to be cancer). This would lead to unneeded biopsies and other tests in many of these women.
The American Cancer Society believes the use of mammograms, MRI (in women at high risk), clinical breast exams, and finding and reporting breast changes early, according to the recommendations outlined above,offers women the best chance to reduce their risk of dying from breast cancer. This combined approach is clearly better than any one exam or test alone. Without question, breast physical exam without a mammogram would miss the opportunity to detect many breast cancers that are too small for a woman or her doctor to feel but can be seen on mammograms. Although mammograms are a sensitive screening method, a small percentage of breast cancers do not show up on mammograms but can be felt by a woman or her doctors.
For women at high risk of breast cancer, such as those with BRCA gene mutations or a strong family history, both MRI and mammogram exams of the breast are recommended.
Mammograms
A mammogram is an x-ray of the breast. A diagnostic mammogram is used to diagnose breast disease in women who have breast symptoms or an abnormal result on a screening mammogram. Screening mammograms are used to look for breast disease in women who are asymptomatic; that is, they appear to have no breast problems. Screening mammograms usually take 2 views (x-ray pictures taken from different angles) of each breast. For some patients, such as women with breast implants, more pictures may be needed to include as much breast tissue as possible. Women who are breast-feeding can still get mammograms, although these are probably not quite as accurate because the breast tissue tends to be dense.
Although breast x-rays have been done for more than 70 years, the modern mammogram has only existed since 1969. That was the first year x-ray units specifically for breast imaging were available. Modern mammogram equipment designed for breast x-rays uses very low levels of radiation, usually a dose of about 0.1 to 0.2 rads per picture (a rad is a measure of radiation dose).
Strict guidelines ensure that mammogram equipment is safe and uses the lowest dose of radiation possible. Many people are concerned about the exposure to x-rays, but the level of radiation used in modern mammograms does not significantly increase the risk for breast cancer.
To put dose into perspective, if a woman with breast cancer is treated with radiation, she will receive around 5,000 rads. If she had yearly mammograms beginning at age 40 and continuing until she was 90, she will have received 20 to 40 rads. For a mammogram, the breast is pressed between 2 plates to atten and spread the tissue. Although this may be uncomfortable for a moment, it is necessary to produce a good, readable mammogram. The compression only lasts a few seconds. The entire procedure for a screening mammogram takes about 20 minutes.
This procedure produces a black and white image of the breast tissue either on a large sheet of film or as a digital computer image that is read, or interpreted, by a radiologist (a doctor trained to interpret images from x-rays, ultrasound, MRI, and related tests). Some advances in technology, such as digital mammography, may help doctors read mammograms more accurately. They are described here.
What the doctor looks for on your mammogram
The doctor reading the films will look for several types of changes:
Calcifications are tiny mineral deposits within the breast tissue, which look like small white spots on the films. They may or may not be caused by cancer. There are 2 types of calcifications:
Macrocalcifications are coarse (larger) calcium deposits that are most likely changes in the breasts caused by aging of the breast arteries, old injuries, or in ammation. These deposits are related to non-cancerous conditions and do not require a biopsy. Macrocalcifications are found in about half the women over 50, and in about 1 of 10 women under 50.
Microcalcifications are tiny specks of calcium in the breast. They may appear alone or in clusters. Microcalcifications seen on a mammogram are of more concern, but still usually do not mean that cancer is present. The shape and layout of microcalcifications help the radiologist judge how likely it is that cancer is present. If the calcifications look suspicious for cancer, a biopsy will be done.
A mass, which may occur with or without calcifications, is another important change seen on mammograms. Masses can be many things, including cysts (non-cancerous, fluid-filled sacs) and non-cancerous solid tumors (such as broadenomas), but they could also be cancer. Masses that are not cysts usually need to be biopsied. A cyst and a tumor can feel alike on a physical exam. They can also look the same on a mammogram. To confirm that a mass is really a cyst, a breast ultrasound is often done. Another option is to remove (aspirate) the fluid from the cyst with a thin, hollow needle.
If a mass is not a simple cyst (that is, if it is at least partly solid), then you may need to have more imaging tests. Some masses can be watched with periodic mammograms, while others may need a biopsy. The size, shape, and margins (edges) of the mass help the radiologist determine if cancer is present.
Having your previous mammograms available for the radiologist is very important. They can be helpful to show that a mass or calcification has not changed for many years. This would mean that it is probably a benign condition and a biopsy is not needed.
Limitations of mammograms
A mammogram cannot prove that an abnormal area is cancer. To confirm whether cancer is present, a small amount of tissue must be removed and looked at under a microscope. This procedure, called a biopsy, is described here.
You should also be aware that mammograms are done to find breast cancer that cannot be felt. If you have a breast lump, you should have it checked by your doctor and consider having it biopsied even if your mammogram result is normal. For some women, such as those with breast implants, additional pictures may be needed. Breast implants make it harder to see breast tissue on standard mammograms, but additional x-ray pictures with implant displacement and compression views can be used to more completely examine the breast tissue.
Mammograms are not perfect at finding breast cancer. They do not work as well in younger women, usually because their breasts are dense, and can hide a tumor. This may also be true for pregnant women and women who are breast-feeding. Since most breast cancers occur in older women, this is usually not a major concern.
However, this can be a problem for young women who are at high risk for breast cancer (due to gene mutations, a strong family history of breast cancer, or other factors) because they often develop breast cancer at a younger age. For this reason, the American Cancer Society now recommends MRI scans in addition to mammograms for screening in these women. (MRI scans are described below.)
More information on these tests is available here and the separate American Cancer Society document, Mammograms and Other Breast Imaging Procedures.
What to expect when you have a mammogram
- To have a mammogram you must undress above the waist. The facility will give you a wrap to wear.
- A technologist will be there to position your breasts for the mammogram. Most technologists are women. You and the technologist are the only ones in the room during the mammogram. To get a high-quality mammogram picture with excellent image quality, it is necessary to atten the breast slightly. A technologist places the breast on the mammogram machine’s lower plate, which is made of metal and has a drawer to hold the x-ray film or the camera to produce a digital image. The upper plate, made of plastic, is lowered to compress the breast for a few seconds while the picture is taken.
- The whole procedure takes about 20 minutes. The actual breast compression only lasts a few seconds.
- You will feel some discomfort when your breasts are compressed, and for some women compression can be painful. Try not to schedule a mammogram when your breasts are likely to be tender, as they may
- be just before or during your period.
- All mammogram facilities are now required to send your results to you within 30 days. Generally, you will be contacted within 5 working days if there is a problem with the mammogram.
- Only 2 to 4 mammograms of every 1,000 lead to a diagnosis of cancer. About 10 % of women who have a mammogram will require more tests, and the majority will only need an additional mammogram. Don’t panic if this happens to you. Only 8 % to 10 % of those women will need a biopsy, and most (80%) of those biopsies will not be cancer.
- If you are a woman aged 40 or over, you should get a mammogram every year. You can schedule the next one while you’re at the facility and/or request a reminder.
Tips for having a mammogram
The following are useful suggestions for making sure that you will receive a quality mammogram:
- If it is not posted visibly near the receptionist’s desk, ask to see the FDA certificate that is issued to all facilities that offer mammography. The FDA requires that all facilities meet high professional standards of safety and quality in order to be a provider of mammography services. A facility may not provide mammography without certification.
- Use a facility that either specializes in mammography or does many mammograms a day.
- If you are satisfied that the facility is of high quality, continue to go there on a regular basis so that your mammograms can be compared from year to year.
- If you are going to a facility for the first time, bring a list of the places, dates of mammograms, biopsies, or other breast treatments you have had before.
- If you have had mammograms at another facility, you should make every attempt to get those mammograms to bring with you to the new facility (or have them sent there) so that they can be compared to the new ones.
- On the day of the exam don’t wear deodorant or antiperspirant. Some of these contain substances that can interfere with the reading of the mammogram by appearing on the x-ray film as white spots.
- You may find it easier to wear a skirt or pants, so that you’ll only need to remove your blouse for the exam.
- Schedule your mammogram when your breasts are not tender or swollen to help reduce discomfort and to ensure a good picture. Try to avoid the week just before your period.
- Always describe any breast symptoms or problems that you are having to the technologist who is doing the mammogram. Be prepared to describe any medical history that could affect your breast cancer risk such as surgery, hormone use, or family or personal history of breast cancer.
- Discuss any new findings or problems in your breasts with your doctor or nurse before having a mammogram.
- If you do not hear from your doctor within 10 days, do not assume that your mammogram was normal call your doctor or the facility.
Help with mammogram costs
Medicare, Medicaid, and most private health insurance plans cover mammogram costs or a percentage of them. Low-cost mammograms are available in most communities. Call 1-800-227-2345 for information aboutfacilities in your area.
Breast cancer screening is now more available to medically underserved women through the National Breast and Cervical Cancer Early Detection Program (NBCCEDP). This program provides breast and cervical cancer early detection testing to women without health insurance for free or at very low cost. Although the program is administered within each state, the Centers for Disease Control and Prevention (CDC) provide matching funds and support to each state program. Each state’s Department of Health has information on how to contact the nearest program.
The program is only designed to provide screening. But if a cancer is discovered, it will cover further diagnostic testing and a surgical consultation. The Breast and Cervical Cancer Prevention and Treatment Act gives states Medicaid funds to pay for treating breast and cervical cancers that are detected through the NBCCEDP. This helps women focus their energies on fighting their disease, instead of worrying about how to pay for treatment. All states participate in this
rogram.
To learn more about these programs, please contact the CDC at 1-800-CDC INFO (1-800-232-4636) or
online.
Clinical breast exam
A clinical breast exam (CBE) is an exam of your breasts by a health care professional, such as a doctor, nurse practitioner, nurse, or doctor’s assistant. For this exam, you undress from the waist up. The health care professional will rst look at your breasts for abnormalities in size or shape, or changes in the skin of the breasts or nipple. Then, using the pads of the fingers, the examiner will gently feel (palpate) your breasts.
Special attention will be given to the shape and texture of the breasts, location of any lumps, and whether such lumps are attached to the skin or to deeper tissues. The area under both arms will also be examined. The CBE is a good time for women who don’t know how to examine their breasts to learn the proper technique from their health care professionals. Ask your doctor or nurse to teach you and watch your technique.
Breast awareness and self exam
Beginning in their 20s, women should be told about the benefits and limitations of breast self-exam (BSE). Women should know how their breasts normally look and feel and report any new breast changes to a health professional as soon as they are found. Finding a breast change does not necessarily mean there is a cancer. A woman can notice changes by being aware of how her breasts normally look and feel and by feeling her breasts for changes (breast awareness), or by choosing to use a step-by-step approach (see below) and using a specific schedule to examine her breasts.
If you choose to do BSE, the information below is a step-by-step approach for the exam. The best time for a woman to examine her breasts is when the breasts are not tender or swollen. Women who examine their breasts should have their technique reviewed during their periodic health exams by their health care professional.
Women with breast implants can do BSE, too. It may be helpful to have the surgeon help identify the edges of the implant so that you know what you are feeling. There is some thought that the implants push out the breast tissue and may actually make it easier to examine.
Women who are pregnant or breast-feeding can also choose to examine their breasts regularly. It is acceptable for women to choose not to do BSE or to do BSE once in a while. Women who choose not to do BSE should still be aware of the normal look and feel of their breasts and report any changes to their doctor right away.
How to examine your breasts
- Lie down and place your right arm behind your head. The exam is done while lying down, not standing up. This is because when lying down the breast tissue spreads evenly over the chest wall and is as thin as possible, making it much easier to feel all the breast tissue. Use the finger pads of the 3 middle fingers on your left hand to feel for lumps in the right breast. Use overlapping dime-sized circular motions of the finger pads to feel the breast tissue.
- Use 3 different levels of pressure to feel all the breast tissue. Light pressure is needed to feel the tissue closest to the skin; medium pressure to feel a little deeper; and firm pressure to feel the tissue closest to the chest and ribs. It is normal to feel a firm ridge in the lower curve of each breast, but you should tell your doctor if you feel anything else out of the ordinary. If you’re not sure how hard to press, talk with your doctor or nurse. Use each pressure level to feel the breast tissue before moving on to the next spot.
- Move around the breast in an up and down pattern starting at an imaginary line drawn straight down your side from the underarm and moving across the breast to the middle of the chest bone (sternum or breastbone). Be sure to check the entire breast area going down until you feel only ribs and up to the neck or collar bone (clavicle).
- There is some evidence to suggest that the up-and-down pattern (sometimes called the vertical pattern) is the most effective pattern for covering the entire breast, without missing any breast tissue.
- Repeat the exam on your left breast, putting your left arm behind your head and using the finger pads of your right hand to do the exam.
- While standing in front of a mirror with your hands pressing firmly down on your hips, look at your breasts for any changes of size, shape, contour, or dimpling, or redness or scaliness of the nipple or breast skin. (The pressing down on the hips position contracts the chest wall muscles and enhances any breast changes.)
- Examine each underarm while sitting up or standing and with your arm only slightly raised so you can easily feel in this area. Raising your arm straight up tightens the tissue in this area and makes it harder to examine.
- This procedure for doing breast self exam is different from previous recommendations. These changes represent an extensive review of the medical literature and input from an expert advisory group. There is evidence that this position (lying down), the area felt, pattern of coverage of the breast, and use of different amounts of pressure increase a woman’s ability to find abnormal areas.
Magnetic resonance imaging (MRI)
For certain women at high risk for breast cancer, screening MRI is recommended along with a yearly mammogram. It is not generally recommended as a screening tool by itself, because although it is a sensitivetest, it may still miss some cancers that mammograms would detect.
MRI scans use magnets and radio waves (instead of x-rays) to produce very detailed, cross-sectional images of the body. The most useful MRI exams for breast imaging use a contrast material (gadolinium) that is injected into a vein in the arm before or during the exam. This improves the ability of the MRI to clearly show breast tissue details.
Although MRI is more sensitive in detecting cancers than mammograms, it also has a higher false-positive rate (where the test finds something that turns out not to be cancer), which results in more recalls and biopsies. This is why it is not recommended as a screening test for women at average risk of breast cancer, as it would result in unneeded biopsies and other tests in a large portion of these women.
Just as mammography uses x-ray machines that are specially designed to image the breasts, breast MRI also requires special equipment. Breast MRI machines produce higher quality images than MRI machines designed for head, chest, or abdominal scanning. However, many hospitals and imaging centers do not have dedicated breast MRI equipment available. It is important that screening MRIs be done at facilities that can perform an MRI-guided breast biopsy. Otherwise, the entire scan will need to be repeated at another facility when the biopsy is done.
MRI is more expensive than mammography. Most major insurance companies will likely pay for these screening tests if a woman can be shown to be at high risk, but it’s not yet clear if all companies will do so. At this time there are concerns about costs of and limited access to high-quality MRI breast screening services for women at high risk of breast cancer.
Breast Cancer Screening Recommendations from the American Cancer Society
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

Can Breast Cancer Be Detected Early?

CNN Airs News Story on Male Breast Cancer at Camp Lejeune
CNN Airs News Story on Male Breast Cancer at Camp Lejeune July 07, 2020 Share on Facebook Twitter Linkedin Author: Pam Stephan, About.com Guide to Breast Cancer What is male breast cancer? Mike Partain, male breast cancer survivor and former resident of Camp Lejeune, is back in the news again. Tune in to CNN on […]

Breast Cancer Reconstruction & Health Care Reform – What It Means For You
Breast Cancer Reconstruction & Health Care Reform – What It Means For You July 07, 2020 Share on Facebook Twitter Linkedin Author: Dr. Sharon Lacey What does health care reform mean for patients with breast cancer and how will it affect you? Well, it could mean… Even though you or your loved one could benefit […]

Breast Reconstruction – Breast Cancer Patients Denied Choice After Mastectomy
Breast Reconstruction – Breast Cancer Patients Denied Choice After Mastectomy July 07, 2020 Share on Facebook Twitter Linkedin Author: Dr. Minas Chrysopoulo Are there breast reconstruction options other than implants? Despite the increase of breast reconstruction procedures performed after mastectomy in 2008, nearly 70 percent of women who are eligible for the procedure are not […]

Mammograms and MRI after Breast Reconstruction – Are They Needed?
Mammograms and MRI after Breast Reconstruction – Are They Needed? July 07, 2020 Share on Facebook Twitter Linkedin Author: Dr. Minas Chrysopoulo “Do I still need to have mammograms after my breast reconstruction?” I’m asked this question quite often. Surprisingly, there is no evidence-based consensus on this among breast cancer physicians. Recommendations range from “no need […]

Is there a Place For Breast Reconstruction in Metastatic Breast Cancer?
Is there a Place For Breast Reconstruction in Metastatic Breast Cancer? July 07, 2020 Share on Facebook Twitter Linkedin Author: Dr. Minas Chrysopoulo Can I still have Breast Reconstruction if I have Metastatic Breast Cancer? Traditional medical opinion states that patients with metastatic breast cancer are not candidates for breast reconstruction. Once metastases are diagnosed […]

Impact of Radiation on Breast Reconstruction Surgery
Impact of Radiation on Breast Reconstruction Surgery July 07, 2020 Share on Facebook Twitter Linkedin Author: Dr. Minas Chrysopoulo Can radiation therapy impact breast reconstruction results? Radiation therapy is often recommended as part of breast cancer treatment. Patients undergoing lumpectomy receive radiation routinely once they’ve healed from surgery. Some mastectomy patients also need radiation after […]
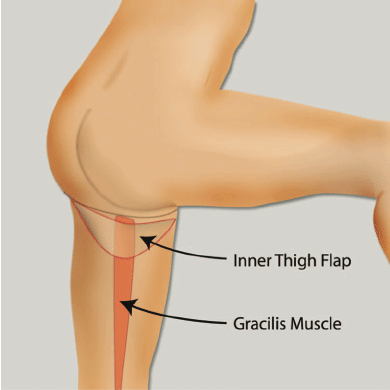
TUG Flap Restores Breast After Mastectomy With Thigh Lift Bonus
TUG Flap Restores Breast After Mastectomy With Thigh Lift Bonus July 07, 2020 Share on Facebook Twitter Linkedin What is TUG flap breast reconstruction? San Antonio, TX (PRWEB) February 23, 2009 – Plastic, Reconstructive & Microsurgical Associates (PRMA) of South Texas, a leading breast reconstruction surgery practice in San Antonio, is now offering women the […]
Breast Reconstruction after Mastectomy – Breast Reconstruction Specialist Radio Interview
Breast Reconstruction after Mastectomy – Breast Reconstruction Specialist Radio Interview July 07, 2020 Share on Facebook Twitter Linkedin What are the cutting edge breast reconstruction options currently available? It was an absolute pleasure to talk to DeLeon and Travis on “DeLeon Dialogue” last night. Breast cancer survivor DeLeon and cervical cancer survivor Travis talk frankly with […]

When Should You Consider Prophylactic Mastectomy of The Non-Cancer Breast?
When Should You Consider Prophylactic Mastectomy of The Non-Cancer Breast? July 07, 2020 Share on Facebook Twitter Linkedin When Should You Consider Prophylactic Mastectomy of The Non-Cancer Breast? Having breast cancer in one breast increases a woman’s chances of getting breast cancer in the second breast at some point. Unless the patient is “high risk” […]


No Comments