
- 2 Comments
- PRMA Plastic Surgery
July 17, 2020
Does prophylactic mastectomy and breast reconstruction impact patients’ intimacy?
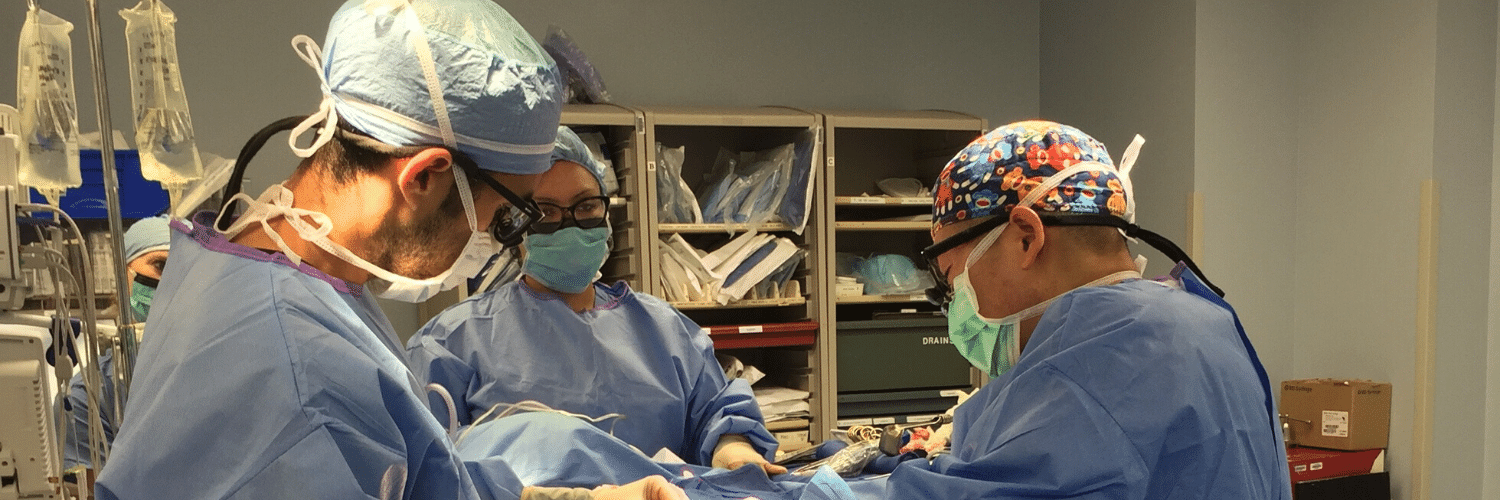
With growing knowledge of genetic mutations and their association with an increased risk of breast cancer, more women are choosing to undergo risk reducing mastectomy and breast reconstruction. This growing trend led researchers to examine what factors influence a patient’s intimate life and overall satisfaction with their breast reconstruction outcomes.
Choosing to undergo a prophylactic mastectomy is a major life-changing decision and can be a good option for patients who are at high risk of developing breast cancer. In certain situations, prophylactic mastectomy can reduce the risk of breast cancer by 90%-95%.
Breast reconstruction is also an option following preventative mastectomy and can be performed using implants or the patient’s own tissue. Regardless of the reconstructive procedure performed, changes in breast sensation and appearance may impact a patient’s intimate life and overall satisfaction with their final results.
A study published in the International Journal of Behavioral Medicine took a closer look at what factors influenced patients’ satisfaction with their reconstructed breasts and intimacy following bilateral prophylactic mastectomy.
The study followed 26 women and concluded satisfaction appeared to be influenced by realistic outcome expectations and communication with others. Women who liked their breasts pre-surgery appeared less satisfied with their reconstructed breasts post-surgery, and women who disliked their breasts before surgery were more satisfied with their reconstructed breasts. Women with unrealistic expectations concerning the look and feel of their reconstructed breasts were often unhappy with their reconstructed breasts and felt they did not meet their expectations
So, what’s the take home message?
It is crucial for surgeons and patients to have honest discussions regarding patient wishes and realistic expectations. This is called Shared Decision Making and we believe it is the most important aspect of patient centered health care! Patients and their doctors should work together to make the decisions for individualized care. Time should be taken to discuss ALL options and the pros and cons of each before creating a surgery plan. It is our belief at PRMA that each patient is unique, and as such, no two breast reconstruction journeys will be alike.
Although reconstructive techniques have come a long way, it is important for patients to understand final results will not always look or feel like what mother nature provided. For example, during the prophylactic mastectomy, nerves supplying feeling to the breast will be cut. This results in a lack of sensation or numbness to the breast. For patients choosing to have tissue-based reconstruction (like the DIEP flap), sensory nerve reconstruction can be performed and can help restore sensation to the breast. Unfortunately, this is not an option for implant reconstruction patients at this time.
Regardless of the procedure being performed, patients should know more than one procedure is typically required for optimal cosmetic results. Referred to as the “Revision Stage” or “Stage 2,” this procedure is designed to fine-tune the reconstructed breast(s) in order to improve the overall cosmetic appearance.
Women undergoing prophylactic mastectomy and breast reconstruction have many options available to them today. By understanding patient needs and discussing realistic expectations, overall satisfaction with reconstruction results and intimacy can be achieved.
Read patient success stories here
Author: Dr. Minas Chrysopoulo and Courtney Floyd
A study published in Plastic and Reconstructive Surgery examined the abdominal recovery rates and patient satisfaction after breast reconstruction with different abdominal flaps: the DIEP, SIEA and muscle-sparing free TRAM.
Leave Comment

I had the DIEP procedure. At the time, 2006, there was no talk of nerve reconstruction. Would that be a consideration now? Are the nerves still in there and could they be connected?
Mary
July 21,2020

Great question Mary. Sadly, after the tissue has been transplanted to the chest, further sensory nerve reconstruction cannot be performed at this time.
PRMA Plastic Surgery
July 21,2020
Sign Up for Our Monthly Newsletter
Continue Reading

Breast Reconstruction Surgery and Your Period
Breast Reconstruction Surgery and Your Period December 02, 2020 Share on Facebook Twitter Linkedin During our pre-operative appointment with patients, a topic that occasionally arises is menstrual cycles. It is completely normal for women to experience changes with their periods throughout breast cancer treatments. These can be temporary or permanent. Periods can be unpredictable following […]

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap September 08, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]
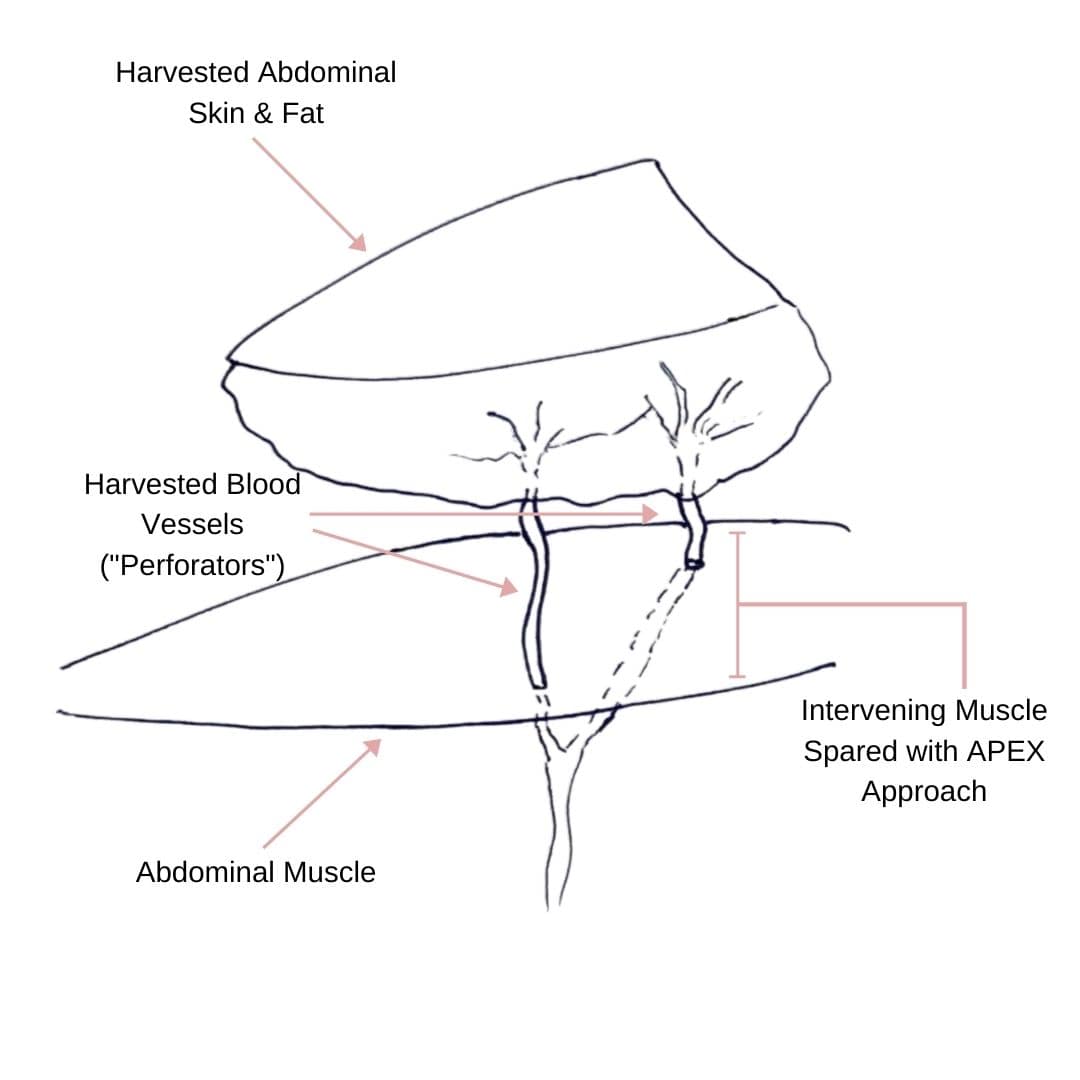
Comparing APEX Flap and DIEP Flap Breast Reconstruction
Comparing APEX Flap and DIEP Flap Breast Reconstruction August 10, 2020 Share on Facebook Twitter Linkedin We have been receiving numerous inquiries about the “APEX flap” recently. Patients want to know what it is and how it differs from the DIEP flap. APEX is an acronym that stands for “Abdominal Perforator Exchange”. Many patients believe […]
Monitoring the Health of Your Flap During & After Surgery
Monitoring the Health of Your Flap During & After Surgery July 21, 2020 Share on Facebook Twitter Linkedin Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap. During this procedure, surgeons transplant skin […]
COVID-19 and the Impact on Cancer Patient’s Mortality
COVID-19 and the Impact on Cancer Patient’s Mortality July 21, 2020 Share on Facebook Twitter Linkedin There is still so much we do not know about COVID-19. Likewise, there is little known about how this disease impacts mortality for cancer patients. A study published in The Lancet evaluated and characterized the outcomes of patients with cancer […]

Breast Cancer Recurrence Risk Does Not Increase Following DIEP Flap Breast Reconstruction
PRMA Patient Shares Her Experience with Hidden Scar Mastectomy and Breast Reconstruction

Mary
I had the DIEP procedure. At the time, 2006, there was no talk of nerve reconstruction. Would that be a consideration now? Are the nerves still in there and could they be connected?
PRMA Plastic Surgery
Great question Mary. Sadly, after the tissue has been transplanted to the chest, further sensory nerve reconstruction cannot be performed at this time.