
- 3 Comments
- PRMA Plastic Surgery
What are common breast cancer misconceptions?
We welcome guest blogger Sheryl Kraft, contributor on Huffington Post and author of two of my favorite blogs, healthywomen.org and mysocalledmidlife.net.
October may be breast cancer awareness month – but really, every month is about breast cancer; it’s never far from my consciousness. I’m reminded of how the disease touched me over 20 years ago when I get dressed every morning. I’m reminded how the disease steals lives when, each January and October, I would have been toasting to another year growing old together with my two closest friends who are no longer in this world because they were part of the cruel statistics. I’m reminded that, despite lots of advances in medical screening, diagnosis and treatment, approximately 12% of women born today will be diagnosed with breast cancer at some time during their lifetime.
There is increased awareness and increased knowledge for sure. But with that, confusion and misinformation still circulate around the issue. Here are some common misconceptions:
1. Breast pain is a symptom of breast cancer.
That’s rarely the case; breast cancer, especially early breast cancer, usually does not cause pain and may exhibit no noticeable symptoms. Most aches, pains or tenderness can be attributed to things like fibrocystic breast changes and the rise and fall of hormones, or a benign fluid-filled sac (a cyst), which can feel firm or squishy and can be aspirated by a doctor to withdraw the fluid causing the pain.
2. You’re only at risk if breast cancer runs in your family.
Only 5 to 10 percent of all breast cancers are hereditary due to mutations in genes associated with the disease. These mutations are more common among certain geographic or ethnic groups, like people of Ashkenazi (central or eastern European) Jewish descent and people of Norwegian, Icelandic or Dutch ancestry. Because they have a shared ancestry over many generations, particular genetic changes can occur more frequently in these groups.
3. Monthly self-exams don’t make a difference.
Despite recent advice discounting the importance of regular breast checks, many experts still believe in them. Mammography, clinical exams, MRIs: they’re reliable screening methods, yet none of them is perfect, so it’s wise to increase your chance of early detection by becoming familiar with your own breasts and reporting any changes, like lumps, swelling, dimpling or discharge to your doctor.
4. Tight, underwire bras cause breast cancer.
This myth started with a husband and wife medical anthropologist team claiming that by wearing tight-fitting bras all day, every day, women inhibited lymphatic drainage, thus causing toxins to become trapped in breast tissue. But scientists discounted this theory in its failure to exclude confounding variables such as the presence in some women of known risk factors for breast cancer such as family history, hormones, age, weight, exercise levels, giving birth over the age of 30 or not having had children.
5. Only women get breast cancer.
Although women do account for the vast majority of breast cancers, men are susceptible, too. With men, their cancers are usually linked to a strong family history or genetic causes and are usually seen in later stages, since men are not typically screened for breast cancer.
6. Older women don’t need to get mammograms.
Since the incidence of breast cancer increases with age, older women should get mammograms indefinitely. The highest incidence of the disease is in women in their 70s. The risk is approximately 1 in 23 for a woman in her 30s; rising to 1 in 8 by the time she is 85.
7. Wearing antiperspirant causes breast cancer.
Parabens, which are used as preservatives in some antiperspirants, do have weak estrogen-like properties. One small study found parabens in samples of tissue from human breast tumors but failed to analyze healthy breast tissue or tissues from other areas of the body (thus failing to demonstrate that parabens are found only in cancerous breast tissue). Subsequent studies have been unable to make a definite connection between parabens and breast cancer. The American Cancer Society says that more research is needed to study this issue.
8. A lump is the only sign of breast cancer.
While a lump may indicate breast cancer or other benign breast conditions, there are other changes that could indicate cancer, like skin irritation or dimpling; swelling, nipple retraction or discharge (other than breast milk); redness, scaliness, or thickening of the nipple or breast skin. Lymph nodes under the arm might swell if the cancer has already spread before a tumor in the breast is even large enough to be felt. And a mammogram can pick up a cancer before any symptom is felt or seen at all.
9. Only your mother’s family history of breast cancer is important.
Your father’s family history is just as important, especially the women on his side of the family. And other cancers in men, like early-onset prostate or colon cancers should be considered when assessing your risk, too.
10. Women with lumpy, fibrocystic breasts are more at risk.
Once thought a factor in increasing your risk, it is no longer seen as a connection. Lumpy breasts do, however, make it more difficult to differentiate normal tissue from cancerous tissue, so ask your doctor if you might be helped further by adding an ultrasound to your mammogram screenings
Sheryl Kraft, Independent Journalist and Blogger
To kick off Breast Cancer Awareness Month we welcome guest blogger Sheryl Kraft, contributor on Huffington Post and author of two of my favorite blogs, healthywomen.org and mysocalledmidlife.net.
Leave Comment

Thank you so much for this. I am going to share it with everyone I know. I underwent a double mastectomy and decided not to have reconstruction but that is just me. This was my second time around with breast cancer. I had no idea there was anything in my left breast, I was going to the doctor because I was a little sore above the lumpectomy scar in the right breast. Thank God I insisted that a mammogram be done on the left also. It was microscopic and I may not have known until it was too late.
Diane
July 20,2020

our church, the clarion call Christian center is hosting a public health fair on saturday, 10-11-14 from 10-1pm to educate the public about breast cancer in men and women and would be honored to have your organization represent in any way. Please bless us by being a blessing to our community and say you can attend.
Linda
July 20,2020

Hey Linda! I would love to chat more with you about the health fair. Please give me a call at 201-692-1181!
PRMA Plastic Surgery
July 20,2020
Sign Up for Our Monthly Newsletter
Continue Reading
A Year in Review at PRMA – 2020
A Year in Review at PRMA – 2020 December 28, 2020 Share on Facebook Twitter Linkedin The COVID-19 global pandemic is an event that has made 2020 a year like no other. It can be hard to feel optimistic or reflect on the good with a year full of unprecedented change. “This past year has […]

Reducing the Risk of Chronic Opioid Use After Breast Reconstruction with ERAS Protocol
Reducing the Risk of Chronic Opioid Use After Breast Reconstruction with ERAS Protocol December 16, 2020 Share on Facebook Twitter Linkedin A study presented at the 2020 San Antonio Breast Cancer Symposium reported that women with breast cancer may be at a high risk of developing a chronic opioid addiction following mastectomy and reconstructive surgery. […]

Hospital Stay After DIEP Flap Breast Reconstruction: What to Expect
Hospital Stay After DIEP Flap Breast Reconstruction: What to Expect December 09, 2020 Share on Facebook Twitter Linkedin Following DIEP flap breast reconstruction, patients are typically in the hospital for about 2-3 days. During that time, patients often wonder what they should expect. Here is what a typical hospital stay for PRMA patients entails… Flap […]

Breast Reconstruction Surgery and Your Period
Breast Reconstruction Surgery and Your Period December 02, 2020 Share on Facebook Twitter Linkedin During our pre-operative appointment with patients, a topic that occasionally arises is menstrual cycles. It is completely normal for women to experience changes with their periods throughout breast cancer treatments. These can be temporary or permanent. Periods can be unpredictable following […]

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap October 22, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]
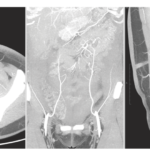
CT Angiogram Before DIEP Flap Reconstruction - Who needs it?
For the Women We Love

Diane
Thank you so much for this. I am going to share it with everyone I know. I underwent a double mastectomy and decided not to have reconstruction but that is just me. This was my second time around with breast cancer. I had no idea there was anything in my left breast, I was going to the doctor because I was a little sore above the lumpectomy scar in the right breast. Thank God I insisted that a mammogram be done on the left also. It was microscopic and I may not have known until it was too late.
Linda
our church, the clarion call Christian center is hosting a public health fair on saturday, 10-11-14 from 10-1pm to educate the public about breast cancer in men and women and would be honored to have your organization represent in any way. Please bless us by being a blessing to our community and say you can attend.
PRMA Plastic Surgery
Hey Linda! I would love to chat more with you about the health fair. Please give me a call at 201-692-1181!