Few Women Have Regrets When Choosing Preventive Mastectomy

Should you have a preventative mastectomy on the non-affected breast to reduce your risk of breast cancer?
Is this for me? If you have been diagnosed with breast cancer in one breast and are considering having the other breast removed to reduce your risk of developing new breast cancer or having cancer coming back, you might want to read this article.
Background and importance of the study: If you have been diagnosed with breast cancer, your risk of developing a new cancer is higher than that of a woman who has never had the disease. The size of this risk varies from person to person because each person has different risk factors. For the average woman who has had breast cancer, the risk of developing new and different breast cancer in the other breast (not a recurrence of the first one) is about 1 % per year. This means a risk of about 10 % over 10 years. Put differently, out of 100 women who have a personal history of the disease, about 10 will get new breast cancer on the other side within 10 years.
The risk of new breast cancer is higher for women who have additional risk factors. If you’ve been diagnosed with breast cancer and also have a strong family history of the disease, your risk is likely to be higher than 1 % a year. If you have a proven genetic abnormality, your risk is even higher. If you have both a strong family history of breast cancer AND a known breast cancer gene abnormality, on top of a personal history of breast cancer, the risk is higher still. The range of higher risk is about 2 % to 5 % per year, depending on all of these factors, plus other things that might affect how an abnormal gene behaves.
Over 10 years, this translates to a risk that ranges from 20 % to 50 %. If you have a personal history of breast cancer plus other risk factors for new breast cancer, it’s important for you to help reduce your risk. You may want to seriously consider extra preventive measures,
including lifestyle changes, medications, and surgery.
Preventive surgery to remove the other breast is a serious option with real benefits and side effects. While removing the breast can substantially reduce your risk of breast cancer, it involves permanent changes that can change your quality of life. The higher your risk of breast cancer, the more likely you are to benefit from preventive surgery. Removal of the breast can decrease the risk of new breast cancer by about 90 %. That’s a big reduction. If your risk is estimated to be 80 %, it could be lowered to about 8 % by preventive breast removal. If your risk is 10 %, it could be lowered to 1 %.
The surgical option of breast removal is called “prophylactic,” which means “preventive.” If you take this step, you are doing something that will significantly reduce your risk for cancer in the future (although there is no guarantee). This option is permanent and irreversible.
Earlier studies have shown that for women with a personal history of breast cancer and other strong risk factors, preventive removal of the other breast (called contralateral mastectomy) reduces their risk of developing new cancer and is associated with improved survival. Up to this point, however, no one had looked at how happy or satisfied women were with their choice.
In this study, the researchers asked women how content they were with their choice to have or not have a preventive mastectomy.
Study design: In this study, the researchers asked 772 women who had a preventive mastectomy and 105 who didn’t have preventive mastectomy how content they were with their choice. All the women had been diagnosed with breast cancer in one breast between 1979 and 1999 at one of six Cancer Research Network health care system centers in the United States. The women were aged 18 to 80.
To determine how content women were with their preventive mastectomy choice, the researchers mailed them a survey that asked questions about:
- quality of life,
- satisfaction with the surgery,
- body image,
- sexual satisfaction,
- depression,
- breast cancer thoughts, and
- health perception.
About 73 % of the surveys were returned, from 519 women who had a preventive mastectomy and 61 women who didn’t. Of those 61 women, 30 had a single mastectomy, and 31 had a lumpectomy. The research was funded by the National Cancer Institute.
Results: Of the 519 women who had a preventive mastectomy, 86.5 % were satisfied with the procedure and had no second thoughts about it, and 76 % were very content with their quality of life. Similarly, of the 61 women who did not have preventive surgery, 75 % were very content with their quality of life.
There was no association between women reporting having a lower quality of life and having had a preventive mastectomy or breast reconstruction, or with the women’s age, race, education, or body mass index. But a lower quality of life WAS linked to:
- poor perception of one’s own general health,
- possible depression,
- unhappiness or self-consciousness about appearance,
- unhappiness with sex life, and
- feeling the need to avoid thoughts of breast cancer.
The results also showed that almost 75 % of the women who didn’t have preventive mastectomy were concerned about breast cancer, compared to 50 % of the women who had preventive surgery.
Conclusions: The researchers concluded that most women who have preventive mastectomy are satisfied with their choice and report having a good quality of life. The women who had preventive mastectomy were less likely than the other women to be concerned about breast cancer. Women who reported having a lower quality of life were more likely to have poor body image, be unhappy with their sex life, possibly be depressed, feel the need to avoid thoughts of breast cancer, and have a poor general health perception.
Take-home message: If you have been diagnosed with breast cancer in one breast and are considering a preventive mastectomy, this study offers strong support that no matter which decision you make, you are likely to be content with that decision later. More than 75 % of women in each group were very content with their quality of life.
Of course, you need to balance the potential benefits of preventive surgery against the side effects. Every woman is unique. How you balance the benefits and side effects in your own situation is very personal.
In general, factors that might make you more likely to choose preventive mastectomy are:
- a strong family history of breast cancer,
- a serious diagnosis of breast cancer in the other breast,
- being very fearful of another cancer,
- lacking confidence in the power of early detection, and
- feeling determined to never go through cancer therapy again.
This wasn’t a randomized study, in which women are assigned to different groups. Every woman made her own decisions, and the women who chose preventive surgery are probably different in many ways from the women who chose not to have this procedure. As a result, comparing the two groups has limited value.
You probably know that we all need to believe in the big decisions we make‚¨”particularly important decisions about our health. But even when we get used to a big decision, it’s normal to have mixed feelings. Although mastectomy can give women more peace of mind, it’s also normal for women to have concerns about their body image and to miss their breast. Also remember that no procedure, even surgery, totally eliminates the risk of cancer. Even when a breast has been removed, cancer can still develop in the area where the breast used to be.
Close follow-up is necessary for all women, even after preventive surgery. You have time to decide. The decision to have preventive surgery is not an emergency. Of course, the decision to have preventive surgery at any age requires much thought and must be made in consultation with your health care team.
SOURCE: Journal of Clinical Oncology; breastcancer.org
Women with breast cancer who are involved in the process of selecting their surgeon are more likely to be treated by more experienced surgeons and in hospitals/centers with established breast cancer programs, according to a study published in the Journal of Clinical Oncology.
Leave Comment
Sign Up for Our Monthly Newsletter
Related News & Press

Few Women Have Regrets When Choosing Preventive Mastectomy for Other Breast
Few Women Have Regrets When Choosing Preventive Mastectomy for Other Breast Share on Facebook Twitter Linkedin Should you have a preventative mastectomy on the non-affected breast to reduce your risk of breast cancer? Is this for me? If you have been diagnosed with breast cancer in one breast and are considering having the other breast […]
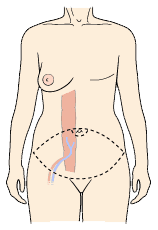
DIEP Flap Surgery And How To Find A DIEP Surgeon
DIEP Flap Surgery And How To Find A DIEP Surgeon Share on Facebook Twitter Linkedin How can I find a DIEP flap breast reconstruction surgeon? Meet PRMA’s award winning DIEP flap surgeons DIEP flap surgery – so why all the hype? If you are a woman facing mastectomy due to breast cancer, one of the decisions […]
Patients Report Improved Quality of Life After DIEP Flap Breast Reconstruction
Patients Report Improved Quality of Life After DIEP Flap Breast Reconstruction June 15, 2020 Share on Facebook Twitter Linkedin Heading2 sed ut perspiciatis unde omnis iste natus Far far away, behind the word mountains, far from the countries Vokalia. Far far away, behind the word mountains, far from the countries Vokalia. Far far away, behind […]
Breast Reconstruction Message Boards, Groups & Forums
Breast Reconstruction Message Boards, Groups & Forums June 15, 2020 Share on Facebook Twitter Linkedin Heading2 sed ut perspiciatis unde omnis iste natus Far far away, behind the word mountains, far from the countries Vokalia. Far far away, behind the word mountains, far from the countries Vokalia. Far far away, behind the word mountains, far […]


No Comments