
- 0 Comments
- PRMA Plastic Surgery
Lymphedema is an abnormal swelling that occurs in the extremities for breast cancer patients. It is related to prior surgery, usually when lymph nodes are removed in the armpit area during an axillary lymph node dissection or a sentinel lymph node biopsy. Much less common in the sentinel lymph node biopsy, but it can occur. The Lymphatic system, which helps control the fluid in the upper extremities, and also helps when immune function is disrupted. When that occurs, it can cause that fluid to build up and cause swelling in the arm area, and we call that lymphedema.
What steps can breast cancer patients take to reduce the risk of lymphedema?
So the first step is to make sure your surgeon is evaluating you for lymphedema, and if you are a high risk patient and you aren’t hearing it from your surgeon, you need to inquire and ask about it. So the high risk patients are those who again have had lymph nodes removed, ten or more lymph nodes is kind of the key number of lymph nodes removed from the armpit area, have had chemo therapy, have had radiation therapy or they are going to get radiation therapy to the chest or to the axillary area or the supraclavicular lymph nodes, or patients who have a BMI of higher than 30 are those patients that are most at risk for developing lymphedema. So the first thing you do is have a discussion with your surgeon and see if you are a patient that fits one of those categories, and if you are its important to get plugged in with a lymphedema therapist to help mitigate some of the potential complications of having those risk factors. With the current situation with COVID-19 and the infections, and patients aren’t able to have the same access to healthcare providers, it’s important to establish a relationship with a lymphedema therapist, or at least communicate with them. A lot of times they can teach you home methods for manual lymphatic drainage that you can do in your house in addition to just maintaining good skin hygiene. Moisture is very important, thankfully we are getting outside the winter time period, but during winter times, or colder climates you can have skin cracks from dry skin with low humidity and maintaining good skin hygiene and moisture with lotions and creams can really help prevent you from having complications such as an infection, which can lead to a lymphedema situation.
What symptoms should patients look out for if they are concerned about being high risk for developing lymphedema?
Good Question. So the most common thing that patients will complain about is a kind of heaviness in the upper extremity. Swelling is what we classically think of when we think of lymphedema clinically, but you know the earlier stage of lymphedema some patients may not have any visible swelling or objective measurement swelling, but they will complain of heaviness or sometimes it’s just kind of a dull ache in the arm area. Some patients will notice that they have kind of a loss of dexterity in their hands, particularly if it’s their dominant hand. For example, a right hand dominant person, and say you know what, my dexterity in my finger, fine movements aren’t what they use to be in this arm and I feel that it is just a little bit odd. Those are kind of the symptoms you should be careful for. Of course swelling if you wear rings, you may notice your rings fit a little tighter than usual. Clothing may also fit a little differently than it would otherwise. Those can all be indications of lymphedema.
If a patient suspects that he or she has lymphedema, what should they do currently?
So again, I think the best course of action would be to reach out to your general surgeon and see if they have a lymphedema therapist that they would refer you to, and depending on if that lymphedema therapist is able to evaluate patients. A lot of things have changed because of the situation that we are in, but they may have some literature that can outline things you can do at home, again, with the self-care, the manual lymphatic drainage are some things you can do at home. There aren’t any good studies on using lymphatic brushes or dry brushing, but these things can be found even online on Amazon. It is something that I routinely recommend to my patients. It can help, and I don’t think it would hurt at all, but it can help stimulate the lymphatic system. It’s a very light brushing on the lymphatic system, on the extremities. It is very superficial, its not in the muscles so its not a massage you would feel the same type of depth of pressure you would in a regular massage of your muscles. The lymphatic system is very superficial in the skin, so if you have the opportunity to get a manual lymphatic drainage by a therapist you’ll notice that they have a very light touch, and I think this dry brushing can also help with that, but it obviously doesn’t replace the professional certified lymphedema therapist with their technique. It is something that can be used as an adjunct particularly during this time period.
What are the treatment options for lymphedema? You mentioned the dry brushing, I guess that is to help with symptoms, but are there actual treatment options for patients diagnosed with lymphedema?
Yes, so first thing is to make sure you are evaluated by a lymphedema therapist to determine if you actually do have lymphedema. Once that’s determined, or if you are very high risk and you are going to see a plastic surgeon, that is one thing to ask the plastic surgeon if they offer any treatments for lymphedema. There are surgical treatments, these are newer treatments. Not many surgeons offer, or are able to do this type of surgery. At PRMA we do specialize in comprehensive restorative breast care, so we do obviously breast reconstruction. We also do lymphatic surgery for patients that have had lymphedema. There are two main treatments, one involves transferring lymph nodes to help replace the lymph nodes that were removed and the other involves Lymphaticovenous Anastomosis or also known as a Lymphaticovenous bypass and that is just a way for us to physically re-route they lymphatic channel to the venous system and it can help bypass the obstruction from the lymph nodes surgery.
Just to kind of wrap it up, for patients who may be interested in seeking an opinion if they are a good candidate for lymphedema surgery during the time of Coronavirus outbreak, and our office being closed currently, can patients reach out to us via telemedicine?
Yes so we take patients from all over the country, even before this pandemic, and we are set up to do virtual consults. We have patients come from other parts of the world and we are able to do a telemedicine evaluation. That is the perfect way for a patient to have a consultation from the comfort of their home without having to venture to a physician’s office. We do an initial intake then we can do a Skype interview type of discussion and see if you are a good candidate for pursuing lymphatic surgery.
What surgical options is PRMA offering for lymphedema?
We do the Lymphaticovenous Anastomosis, or the Lymphaticovenous bypass or LVA. We also do the lymph node transfer. With the lymph node transfer, we are mostly doing that with patients who require breast reconstruction so it is done in conjunction with the breast reconstruction. The LVA surgery is performed as a stand-alone procedure.
Author: Dr. Ramon Garza III and Courtney Floyd
Lymphedema is an abnormal swelling that occurs in the extremities for breast cancer patients. It is related to prior surgery, usually when lymph nodes are removed in the armpit area during an axillary lymph node dissection or a sentinel lymph node biopsy.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

Breast Reconstruction Surgery and Your Period
Breast Reconstruction Surgery and Your Period December 02, 2020 Share on Facebook Twitter Linkedin During our pre-operative appointment with patients, a topic that occasionally arises is menstrual cycles. It is completely normal for women to experience changes with their periods throughout breast cancer treatments. These can be temporary or permanent. Periods can be unpredictable following […]

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap September 08, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]
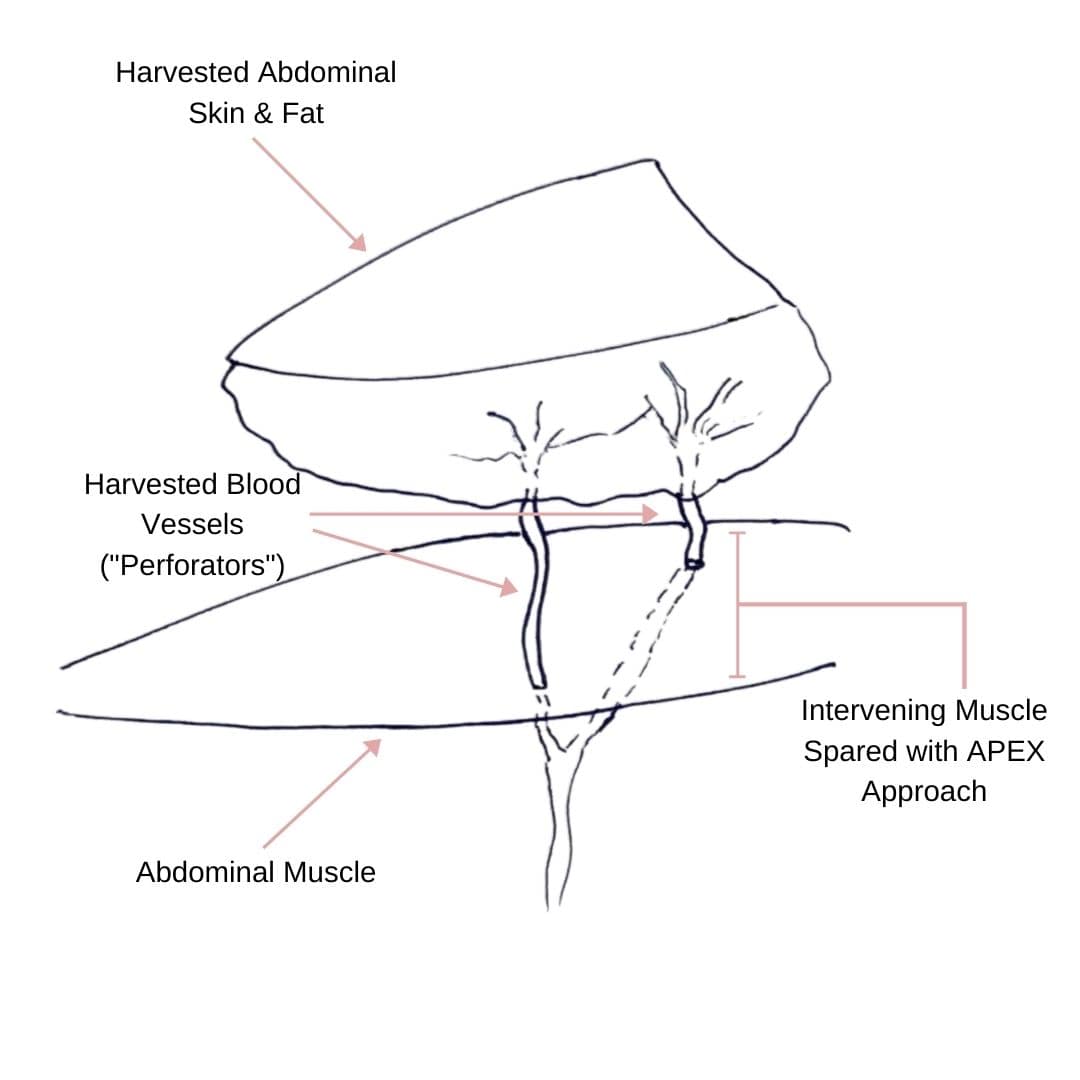
Comparing APEX Flap and DIEP Flap Breast Reconstruction
Comparing APEX Flap and DIEP Flap Breast Reconstruction August 10, 2020 Share on Facebook Twitter Linkedin We have been receiving numerous inquiries about the “APEX flap” recently. Patients want to know what it is and how it differs from the DIEP flap. APEX is an acronym that stands for “Abdominal Perforator Exchange”. Many patients believe […]
Monitoring the Health of Your Flap During & After Surgery
Monitoring the Health of Your Flap During & After Surgery July 21, 2020 Share on Facebook Twitter Linkedin Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap. During this procedure, surgeons transplant skin […]
COVID-19 and the Impact on Cancer Patient’s Mortality
COVID-19 and the Impact on Cancer Patient’s Mortality July 21, 2020 Share on Facebook Twitter Linkedin There is still so much we do not know about COVID-19. Likewise, there is little known about how this disease impacts mortality for cancer patients. A study published in The Lancet evaluated and characterized the outcomes of patients with cancer […]


No Comments