- 0 Comments
- PRMA Plastic Surgery
July 08, 2020
Author: Dr. Steven Pisano
What is involved during vascularized lymph node transfer surgery?
Arm lymphedema (permanent arm swelling) after surgery for breast cancer is a common problem, occurring in 7% of women undergoing sentinel lymph node biopsy and up to about 45% of women undergoing a traditional axillary node dissection. Post-surgical radiation therapy increases the likelihood of upper extremity lymphedema further.
Lymphedema of the upper extremity is characterized by an increase in the circumference of the arm and forearm, pitting (soft) edema (swelling), loss of range of motion at the shoulder and/or elbow, and discomfort. In advance cases the tissues can become markedly swollen, hard, discolored (so called “brawny edema”), and even painful.
Treatment of lymphedema can be divided into non-surgical and surgical options.
The non-surgical treatment includes: range of motion exercises, elevation, “lymphatic” massage, compression garments, intermittent pneumatic compression devices, and multi-layered banding. Non-surgical treatment can be effective in mild to moderate cases. The advantage of non-surgical treatment is that it avoids surgery. The disadvantage is that it may not be definitive in mild to moderate cases and may not be sufficiently effective in advanced cases. Non-surgical methods may be also cumbersome and are usually time-consuming.
Several surgical treatments for arm lymphedema have been described including: lymphatic-to-vascular anastomosis (“LVA” hook-up), liposuction, direct soft tissue excision from the upper extremity, transfer or transplant of autologous (from the patient) tissue to the axilla, and more recently vascularized lymph node transfer.
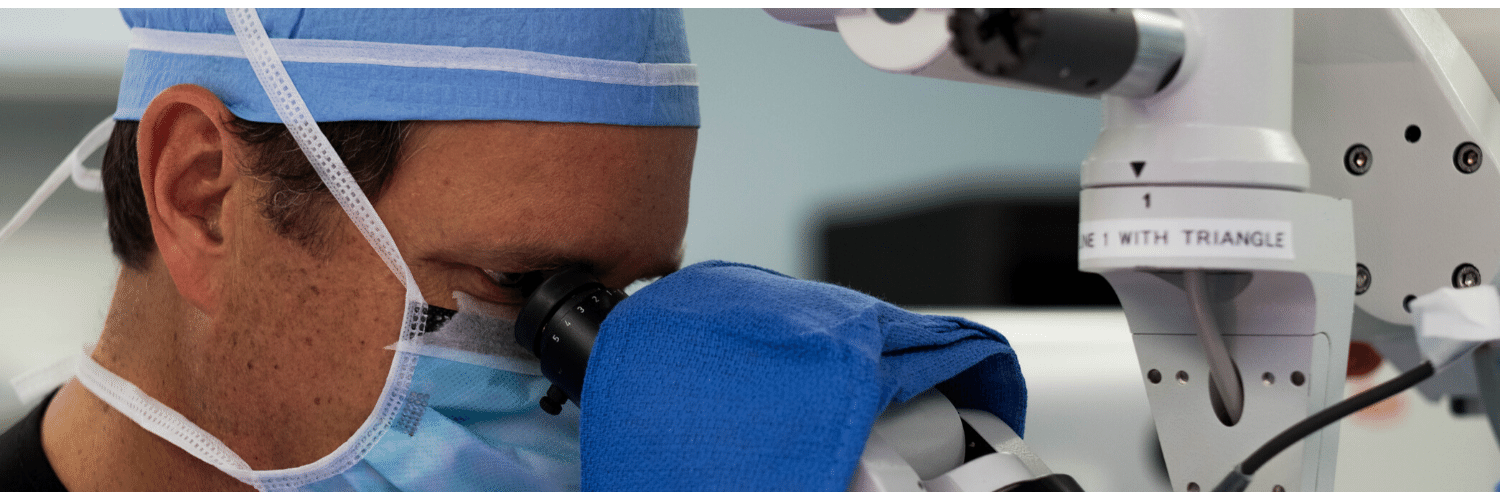
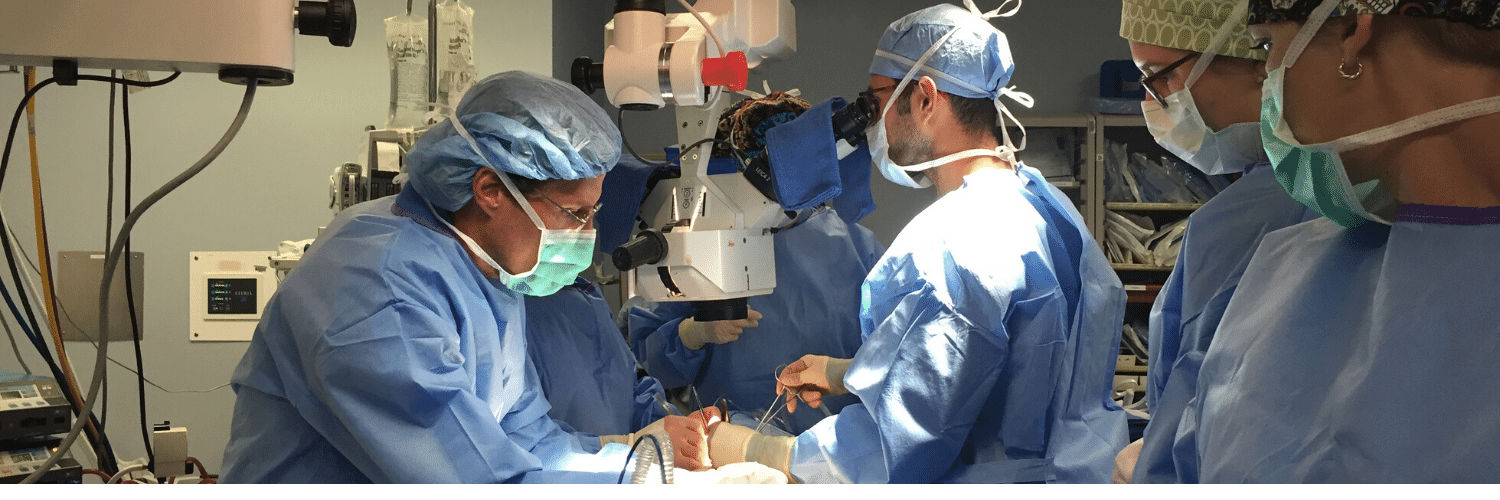
Vascularized lymph node transfer can be performed a couple of ways: lymph nodes can be transplanted at the same time as breast reconstruction with a DIEP flap, or as a stand-alone block of tissue. Both methods can significantly improve lymphedema and recent reports show a high success rate.
Lymph nodes transplanted with a DIEP flap are typically found along the superficial epigastric vein. Groundbreaking work performed at PRMA has also identified nodes along the Deep Inferior Epigastric blood vessels (the same blood vessels that are used in the DIEP flap procedure). Lymph nodes transferred as a stand-alone block of tissue can be harvested from different parts of the body but are most commonly taken from the superficial groin area, using great care to preserve the nodes that drain the leg. Lymph node groups are found along the circumflex iliac vessels or branches off the femoral vessels. The lymph node group is transplanted to the arm. The blood supply to the transplanted lymph nodes is connected to blood vessels in either the wrist, antecubital area (inner elbow), or more commonly the axilla (underarm).
At PRMA we offer the complete spectrum of upper extremity lymphedema treatment. Microsurgery is part of our daily practice and we are proud to offer our patients state-of-the-art reconstructive procedures including the vascularized lymph node transfer and LVA.
Vascularized lymph node transfer has by far shown the best results. The procedure can be performed a couple of ways: lymph nodes can be transplanted at the same time as delayed breast reconstruction with a DIEP flap, or as a stand-alone block of tissue. Both methods can permanently reduce or even eliminate lymphedema and recent reports show a high success rate.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading
Vascularized Lymph Node Transfer Improves Arm Lymphedema after Breast Cancer Surgery

The Five Stages of Cancer Grief
The Five Stages of Cancer Grief July 08, 2020 Share on Facebook Twitter Linkedin Author: Brandy (Korman) Haslam What are the stages of grief during breast cancer? During our Pink Ladies meeting last week, we had the opportunity to meet Lucy Zeigler, PRMA patient and certified professional counselor specializing in grief therapy. Lucy went over […]

Advanced Breast Reconstruction Before and After Photos
Advanced Breast Reconstruction Before and After Photos July 08, 2020 Share on Facebook Twitter Linkedin Author: Brandy (Korman) Haslam Are you interested in breast reconstruction at PRMA and want to see real results of the most advanced breast reconstruction techniques? View our before and after video of patients who had DIEP flap, SIEA flap, LAT […]
Dr. Ochoa Explains Why a Small Portion of Rib is Removed During the DIEP Flap
Dr. Ochoa Explains Why a Small Portion of Rib is Removed During the DIEP Flap July 08, 2020 Share on Facebook Twitter Linkedin Author: Dr. Oscar Ochoa Why is a portion of rib removed during DIEP flap breast reconstruction? The reason why a small portion of the rib is removed (1-2 centimeters) where it meets […]
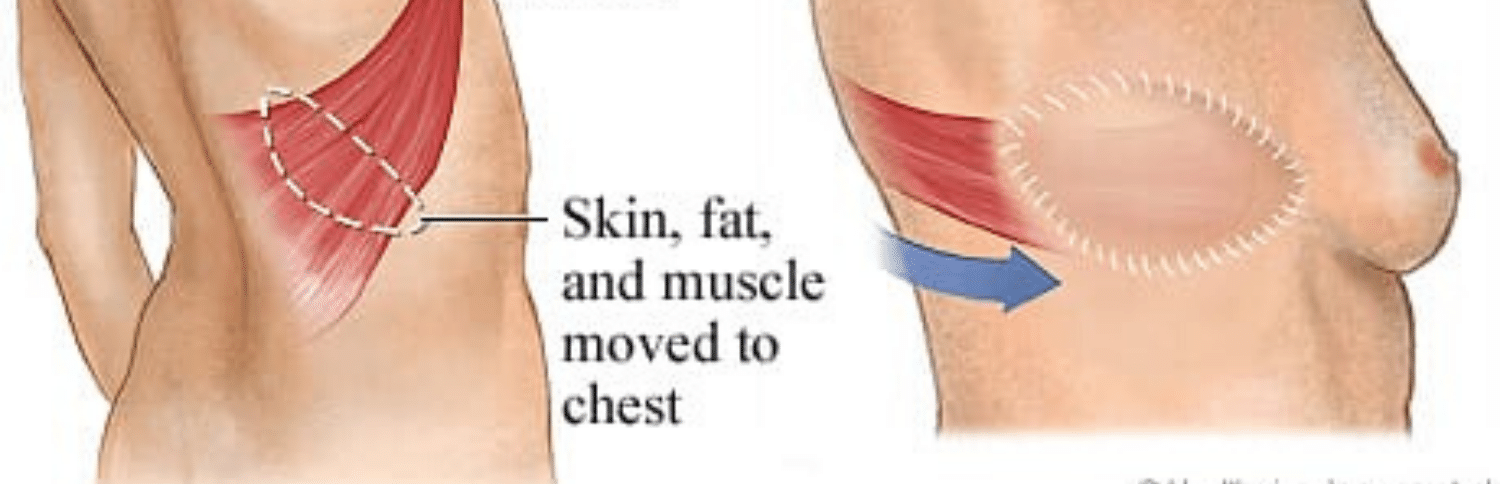
Breast Reconstruction With Latissimus Dorsi Flap
Breast Reconstruction With Latissimus Dorsi Flap July 08, 2020 Share on Facebook Twitter Linkedin Author: Dr. Gary Arishita What is Latissimus flap breast reconstruction? A latissimus (LAT) flap is a procedure where part of the muscle on the back is used to do a reconstruction. A small segment of skin is also included with that […]

Radiation and Breast Reconstruction with Implants
Radiation and Breast Reconstruction with Implants July 08, 2020 Share on Facebook Twitter Linkedin Author: Dr. Gary Arishita Is implant breast reconstruction safe after radiation therapy? It is estimated that in 2013, more then 232,000 women will be diagnosed with invasive breast cancer with over 64,000 being diagnosed with in-situ disease. Of these women, half […]
Keeping Track of Your Medical History
Keeping Track of Your Medical History July 08, 2020 Share on Facebook Twitter Linkedin Author: Brandy (Korman) Haslam Should you keep track of your medical records? If you’ve been diagnosed with breast cancer, chances are you’ve probably seen members of your medical team writing a lot of notes in your chart. These notes are a […]

What is the best timing for breast reconstruction surgery?
What is the best timing for breast reconstruction surgery? July 08, 2020 Share on Facebook Twitter Linkedin Author: Dr. Minas Chrysopoulo What is the best timing for breast reconstruction surgery? In terms of the psycho-social benefits and cosmetic results, breast reconstruction at the same time as the mastectomy is preferred whenever possible. “Immediate reconstruction” is […]

The Five Do’s and Don’ts of Breast Cancer Reconstruction
The Five Do’s and Don’ts of Breast Cancer Reconstruction July 08, 2020 Share on Facebook Twitter Linkedin Author: Dr. Steven Pisano What tips do surgeons offer when planning for breast reconstruction? Do’s: Do seek experience. Breast reconstruction is complicated. Broadly speaking, there are two main categories of breast reconstruction—implant based and tissue based. Within each of […]

Why you shouldn’t smoke if you’re having breast reconstruction
Why you shouldn’t smoke if you’re having breast reconstruction July 08, 2020 Share on Facebook Twitter Linkedin Author: Brandy (Korman) Haslam Is it ok to smoke if you’re having breast reconstruction? It is widely known that tobacco use can cause health issues, but for those patients undergoing breast reconstruction, the effects can be even more […]


No Comments