- 0 Comments
- PRMA Plastic Surgery
How can you prevent capsular contracture?
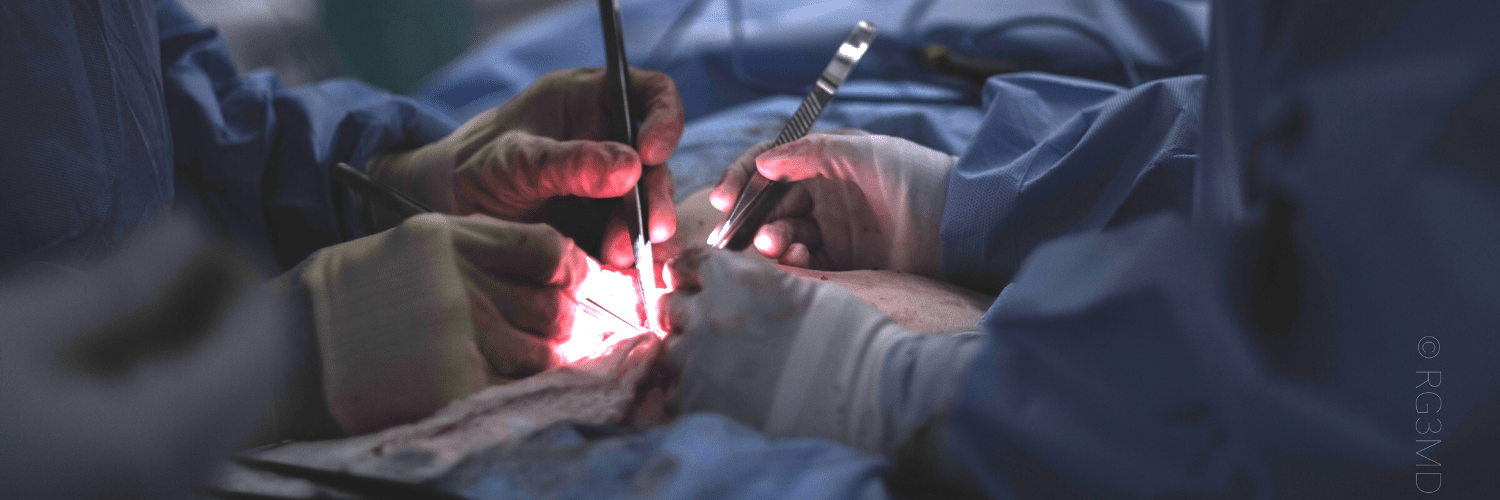
Once capsular contracture is present, methods of treatment are inconsistently effective, making prevention paramount. Known factors such as tissue trauma and bleeding around the implant may be prevented through meticulous surgical technique and verification of absolute hemostasis during implant placement. In particular, surgeons must minimize over-dissection of tissue planes that are non-essential for proper implant placement in order to prevent excessive tissue trauma that may lead to an exaggerated inflammatory process around the implant. Similarly, insertion and removal of an implant multiple times into the implant pocket so as to adjust the pocket dimensions during placement should be eliminated. Not only can such repeated insertion/extraction of an implant cause unnecessary tissue trauma and implant damage, but also increases the potential of implant contamination through contact with bacteria present on the patient’s skin.
Measures to limit implant contamination are simple and cost-effective methods of minimizing capsular contracture. Placement of sterile plastic dressings over the nipples and implant insertion sites as well as exchange of sterile surgical gloves prior to manipulation of an implant are readily available methods that can used in any surgical setting. During placement of silicone gel implants, specialized plastic funnels can be utilized to perform a no-touch insertion technique minimizing contact of the implant with surrounding surfaces. In addition, use of antibiotics given before performing any skin incisions has demonstrated efficacy in decreasing implant contamination. Similarly, irrigation of the implant pocket with antibiotic solution prior to implant placement can decrease the prevalence of implant contamination and subsequent capsular contracture.
Some factors leading to capsular contracture cannot be eliminated, however. External beam radiation, if required as a part of breast cancer treatments, damages the skin and subcutaneous tissue through non-reversible cellular DNA damage that leads to a chronic low-grade inflammatory environment around the implant leading to recurring capsular contracture. In the setting of previous radiation, implant-based breast reconstruction is relatively contraindicated due to a high rate of short-term and long-term complications, namely capsular contracture. Another sporadically occurring condition causing capsular contracture is silicone gel bleed. This phenomenon is caused by hydrolysis of the silicone molecules contained in silicone gel implants over a long period of time. Hydrolysis of the molecules causes the coherent gel to liquefy and slowly diffuse out of an intact silicone shell. Free floating silicone molecules around the implant elicit a low-grade inflammatory response leading to the development of capsular contracture many years following implant placement.
Implant manufacturers have attempted to minimize the prevalence of capsular contracture as well with ongoing research into various components of implant design. Implant surface texturing was one of the initial promising advances aimed at decreasing capsular contracture. By adding micro- and nanotopographical changes to the shell surface through minute undulations and ripples, capsular contracture was minimized likely due to the disoriented alignment of myofibroblasts. Development of more cohesive gels resistant to hydrolysis has been another area of manufacturer research that may hold promise in the future.
Outside of peri-procedural antibiotic use, pharmacologic capsular contracture prevention has been unsuccessful until recently. New studies have reported reduced incidence of capsular contracture with use of a specific class of anti-inflammatory medication called leukotriene inhibitors, such as Singulair®. Leukotrienes are pro-inflammatory derivatives released in response to allergens or other stimuli that result in inflammatory cell activation and infiltration into the site of injury. By blocking the effect of leukotrienes, use of such medications have reduced the prevalence of capsular contracture in reported series. Other anti-inflammatory medications such as synthetic corticosterioid have been used sporadically in the past with variable results warranting controlled studies to determine their efficacy and safety.
Recent advancements in reconstructive medicine have popularized the use of tissue allografts in breast reconstruction. Specifically, acellular dermal matrix (ADM) is widely used in conjunction with implant-based reconstruction to achieve better definition of aesthetically sensitive subunits leading to improved cosmetic outcomes. An unintended benefit of ADM which forms a portion of the periprosthetic capsule is the reported reduced prevalence of capsular contracture. The pathophysiology of this observed characteristic of ADM is a topic of active research but is likely secondary to reduced infiltration of inflammatory cells and fibroblasts within the ADM architecture preventing laminar orientation and contracture. Use of ADM is currently limited to the reconstructive setting or cases of secondary augmentation previously complicated by capsular contracture. Prophylactic use of ADM in primary breast augmentation in order to prevent capsular contracture is not recommended due to the high cost and likely negligible benefit.
Author: Dr. Oscar Ochoa
Recent advancements in reconstructive medicine have popularized the use of tissue allografts in breast reconstruction. Specifically, acellular dermal matrix (ADM) is widely used in conjunction with implant-based reconstruction to achieve better definition of aesthetically sensitive subunits leading to improved cosmetic outcomes.
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading
Monitoring the Health of Your Flap During & After Surgery
Monitoring the Health of Your Flap During & After Surgery July 21, 2020 Share on Facebook Twitter Linkedin Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap. During this procedure, surgeons transplant skin […]
COVID-19 and the Impact on Cancer Patient’s Mortality
COVID-19 and the Impact on Cancer Patient’s Mortality July 21, 2020 Share on Facebook Twitter Linkedin There is still so much we do not know about COVID-19. Likewise, there is little known about how this disease impacts mortality for cancer patients. A study published in The Lancet evaluated and characterized the outcomes of patients with cancer […]

Autologous VS Alloplastic Breast Reconstruction: Patient Reported Satisfaction
Autologous VS Alloplastic Breast Reconstruction: Patient Reported Satisfaction July 21, 2020 Share on Facebook Twitter Linkedin Women who choose to undergo breast reconstruction following a mastectomy have several reconstructive options. Those options can be broken down into two categories – autologous (using your own tissue) and alloplastic (using an implant). Both types of procedures have […]

Dr. Ledoux, BRAVE and Patient Advocate Discuss Breast Reconstruction
Dr. Ledoux, BRAVE and Patient Advocate Discuss Breast Reconstruction July 21, 2020 Share on Facebook Twitter Linkedin Good morning everyone, I am Christine with BRAVE, and I am really excited to introduce our guests today. About a week ago we had Jen Reynolds on as a patient survivor and also the founder of the Pink […]
PRMA Support Spotlight: Pink Warrior Advocates
PRMA Support Spotlight: Pink Warrior Advocates July 21, 2020 Share on Facebook Twitter Linkedin Continuing our weekly support spotlight, we are joined with Jen Reynolds from Pink Warrior Advocates (previously known as Pink Warrior Angels-Hill Country). You can catch the replay of our interview here: Can you please tell us more about your organization? Pink […]

PRMA Support Spotlight: Overcomers
PRMA Support Spotlight: Overcomers July 21, 2020 Share on Facebook Twitter Linkedin We are continuing our weekly support spotlight by featuring the local breast cancer support organization – Overcomers. In this spotlight video we are joined with Genny, a co-founder of Overcomers. What is Overcomers? Overcomers started back in 2015. It was formed for the […]
PRMA Support Spotlight: Susan G. Komen – San Antonio
PRMA Support Spotlight: Susan G. Komen – San Antonio July 21, 2020 Share on Facebook Twitter Linkedin For our Support Spotlight this week we are joined by the local Susan G. Komen organization in San Antonio. How did the local chapter of Susan G. Komen get started? Yes, absolutely, I am so happy to be […]

PRMA Support Spotlight: BRAVE Coalition
PRMA Support Spotlight: BRAVE Coalition July 21, 2020 Share on Facebook Twitter Linkedin In continuation on our weekly Support Spotlight, we are honored to spotlight the BRAVE Coalition! In our interview, we were joined with Christine from BRAVE. Catch the replay here! What is the BRAVE Coalition? BRAVE is a 501 (c)(3) it has been […]

PRMA Support Spotlight: DIEP C Foundation
PRMA Support Spotlight: DIEP C Foundation July 21, 2020 Share on Facebook Twitter Linkedin Today we are honored to spotlight DIEP C Foundation, an amazing organization providing education and resources to empower women and men with information to make an informed decision about options for breast reconstruction after a mastectomy. Can you just kick us of by […]

Numb No More! How PRMA Surgeons Are Restoring Breast Sensation After Mastectomy
Numb No More! How PRMA Surgeons Are Restoring Breast Sensation After Mastectomy July 21, 2020 Share on Facebook Twitter Linkedin Catch the replay of Dr. Chrysopoulo discussing sensory nerve reconstruction and how PRMA surgeons help to restore sensation back to a reconstructed breast following a mastectomy. Can you explain to what causes the loss of sensation to […]


No Comments