
- 0 Comments
- PRMA Plastic Surgery
July 07, 2020
Author: Dr. Minas Chrysopoulo
Can radiation therapy impact breast reconstruction results?
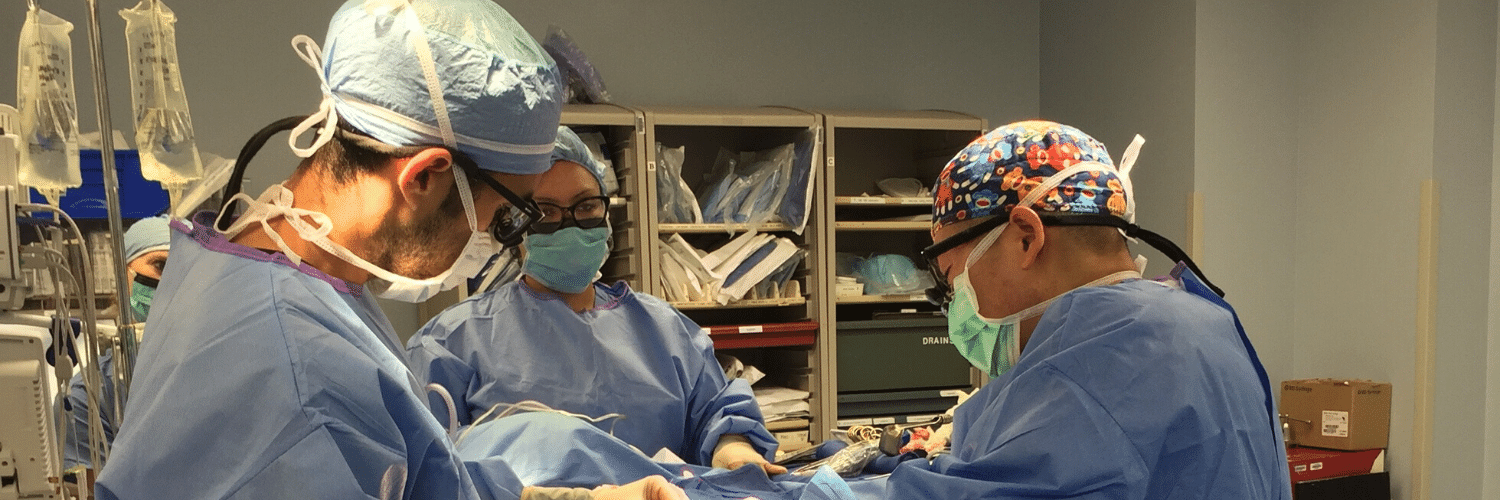
Radiation therapy is often recommended as part of breast cancer treatment. Patients undergoing lumpectomy receive radiation routinely once they’ve healed from surgery. Some mastectomy patients may also need radiation after surgery depending on the characteristics of the tumor. I think it is fair to say that most plastic surgeons are not particularly fond of radiation because of the way it can impact the patient’s tissues, and breast reconstruction results in general.
Nonetheless, it is important to remember that “life comes before breast” and in certain situations, radiation therapy provides very significant benefits from a cancer care perspective, which of course must always remain the priority.
So what’s the problem with radiation therapy (from a plastic surgeon’s perspective)?
For starters, it can cause toughening (fibrosis) and shrinking (contracture) of the patient’s tissue which makes the tissue lose its elasticity and become more tough and rigid. Skin color changes are common, red at first, turning more brown over time. Radiation can also cause burn injuries as well as damage to underlying organs such as the lungs and heart. Radiation therapy technology has improved significantly over the years, and while this has decreased the potential complications considerably, anyone who is facing radiation therapy must discuss all the potential risks with their radiation oncologist beforehand.
Women undergoing lumpectomy are often told that most of their breast will be preserved and that radiation is given “as insurance” to decrease the risk of cancer recurrence. What many women don’t appreciate is that the breast can sometimes end up looking vastly different because of radiation changes, even though they underwent “breast conservation”. This is especially the case if they were small-breasted to begin with.
Not all patients have the same biological response to radiation. Despite the use of protocols, not all radiation oncologists deliver treatment the same way and experience with radiating breast reconstruction patients can vary tremendously. This means results with radiation after breast reconstruction can be quite variable and unpredictable, despite studies that show this is a safe approach in select patients and centers.
Radiation after a tissue (“flap”) reconstruction (eg tram flap, DIEP flap) can cause the reconstructed breast to shrink and harden. Unfortunately, this is a fairly common scenario, especially when the radiation is performed by teams not used to treating reconstruction patients. In rare instances (with heavy radiation doses), new wounds can develop in the reconstructed breast which may need wound care.
Patients who have a mastectomy and flap reconstruction and then have radiation should know that there is a risk of needing further reconstructive surgery to correct changes caused by radiation therapy, and to improve overall breast symmetry. One study found a re-operation rate of almost 30% in patients receiving radiation after TRAM flap reconstruction.
For these reasons, most plastic surgeons still favor delaying flap reconstruction until at least 6 months after completion of radiation treatment.
Tissue expander/implant reconstructions fair even worse with radiation than flaps. The complication rates in this setting are much higher than with tissue reconstructions, including the complete failure of the reconstruction altogether (and removal of the implant).
Some surgeons routinely offer implant reconstructions to patients that are either facing or have already had radiation therapy. Unfortunately, in my experience mixing implants with radiation often ends badly. I will personally only do this in the rare instance that there is no other option, or if the patient strongly prefers to avoid a tissue (flap) reconstruction altogether. The existing literature on breast reconstruction and radiation clearly favors the use of the patient’s own tissue rather than implants in the setting of radiation whenever possible.
So what’s the take-home message?
1) “Breast conservation” can sometimes fall short of the patient’s cosmetic expectations.
2) Breast implants and radiation usually do not mix well.
3) Radiation therapy after a flap reconstruction can significantly impact your reconstruction results, and may require more surgery to improve your overall results, especially if you are in a center that does not routinely care for reconstruction patients. For this reason, most plastic surgeons still advise patients to hold off on their flap reconstruction until after radiation therapy, especially if you are not receiving your treatment in a specialized center.
Radiation therapy is often recommended as part of breast cancer treatment. Patients undergoing lumpectomy receive radiation routinely once they’ve healed from surgery. Some mastectomy patients also need radiation after surgery depending on the characteristics of the tumor. I think it is fair to say that most reconstructive breast surgeons, myself included, are not particularly fond of radiation because of the way it impacts the patient’s tissues (and breast reconstruction in general.)
Leave Comment
Sign Up for Our Monthly Newsletter
Continue Reading

What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery
What Bras and Abdominal Girdles to Wear After Breast Reconstruction Surgery November 17, 2020 Share on Facebook Twitter Linkedin When preparing for breast reconstruction surgery, many patients want to know what types of bras and abdominal girdles they should plan to wear after surgery. Although every surgeon has slightly different preferences, we have put together […]

My 5 DIEP Flap Realities | A Guest Blog From Julie
My 5 DIEP Flap Realities October 28, 2020 Share on Facebook Twitter Linkedin Hi everyone, my name is Julie from It’s a Bosom Thing. I am so happy to be here as a guest blogger and have this opportunity to share with you a few thoughts about life after DIEP Flap Surgery. I was diagnosed […]
PRMA’s BRA Day Virtual Event Recap
PRMA’s BRA Day Virtual Event Recap September 08, 2020 Share on Facebook Twitter Linkedin Yesterday we celebrated Breast Reconstruction Awareness day! Although we missed seeing everyone in person this year, we were still able to spread education and awareness on ALL reconstructive options through our virtual efforts. We were also able to share information on […]

Second Stage DIEP Flap Surgery
Second Stage DIEP Flap Surgery September 08, 2020 Share on Facebook Twitter Linkedin DIEP flap breast reconstruction is typically comprised of at least two stages for the best outcomes. The second stage of surgery is commonly referred to as the “revision” stage and is usually performed about three months after the initial reconstruction. The purpose […]
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them?
If ‘Flaps’ Are Such A Great Breast Reconstruction Option, Why Doesn’t Everyone Get Them? September 08, 2020 Share on Facebook Twitter Linkedin Flap-based breast reconstruction procedures, like the DIEP flap, offer patients a safe, natural implant-alternative option to reconstruction after a mastectomy. Flap surgeries are permanent and are associated with fewer complications after radiation when […]
What is a Skin Island and How is it Used in Breast Reconstruction?
What is a Skin Island and How is it Used in Breast Reconstruction? September 08, 2020 Share on Facebook Twitter Linkedin What is a “skin island”? The term “skin island” is used to describe the remaining visible skin from a transplanted “flap” of tissue. In the setting of DIEP flap breast reconstruction, the skin island […]
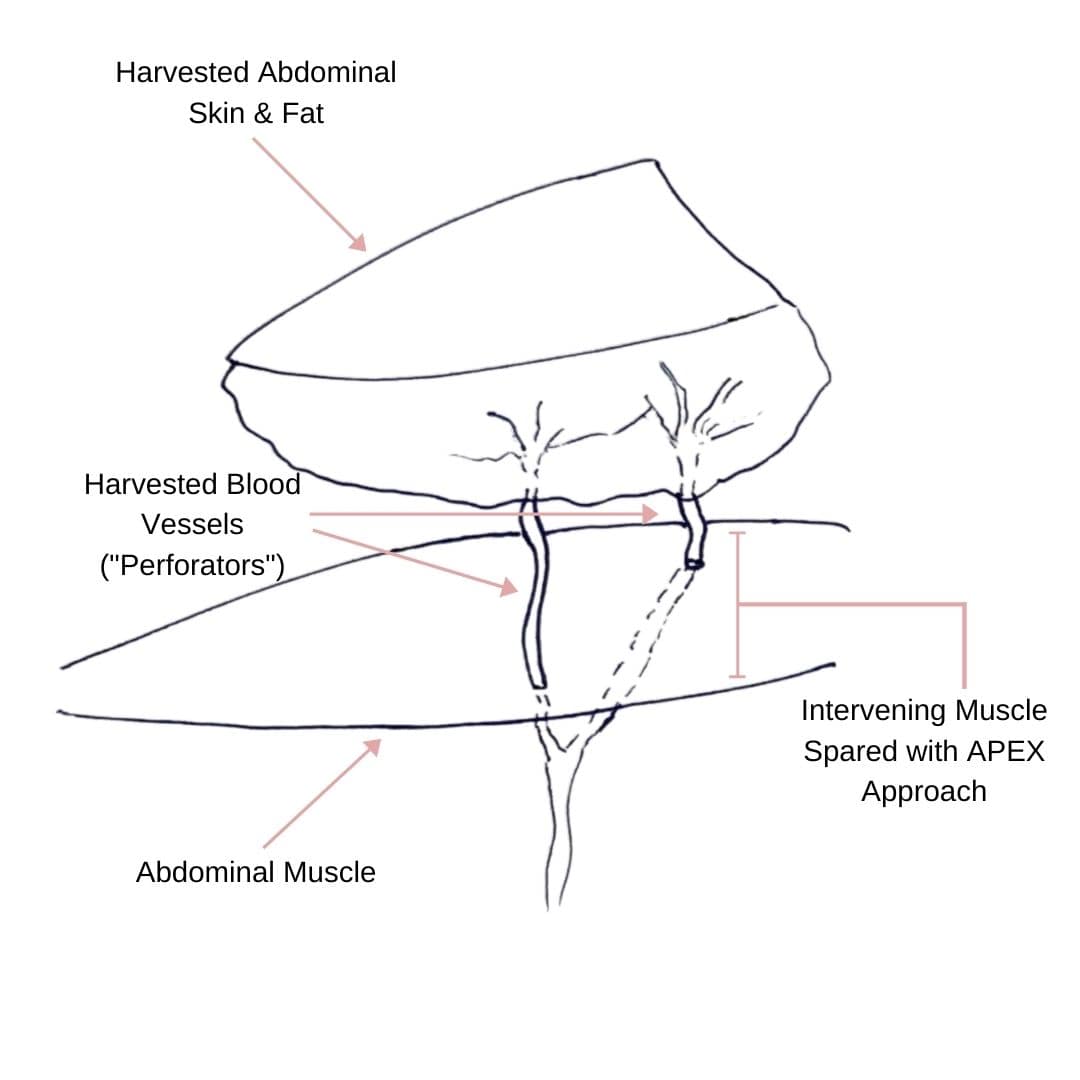
Comparing APEX Flap and DIEP Flap Breast Reconstruction
Comparing APEX Flap and DIEP Flap Breast Reconstruction August 10, 2020 Share on Facebook Twitter Linkedin We have been receiving numerous inquiries about the “APEX flap” recently. Patients want to know what it is and how it differs from the DIEP flap. APEX is an acronym that stands for “Abdominal Perforator Exchange”. Many patients believe […]
Monitoring the Health of Your Flap During & After Surgery
Monitoring the Health of Your Flap During & After Surgery July 21, 2020 Share on Facebook Twitter Linkedin Autologous flap (or tissue) breast reconstruction procedures represent today’s most advanced options for rebuilding a breast(s) following mastectomy. The most commonly performed method of flap-based reconstruction at PRMA is the DIEP flap. During this procedure, surgeons transplant skin […]
COVID-19 and the Impact on Cancer Patient’s Mortality
COVID-19 and the Impact on Cancer Patient’s Mortality July 21, 2020 Share on Facebook Twitter Linkedin There is still so much we do not know about COVID-19. Likewise, there is little known about how this disease impacts mortality for cancer patients. A study published in The Lancet evaluated and characterized the outcomes of patients with cancer […]

Autologous VS Alloplastic Breast Reconstruction: Patient Reported Satisfaction
Autologous VS Alloplastic Breast Reconstruction: Patient Reported Satisfaction July 21, 2020 Share on Facebook Twitter Linkedin Women who choose to undergo breast reconstruction following a mastectomy have several reconstructive options. Those options can be broken down into two categories – autologous (using your own tissue) and alloplastic (using an implant). Both types of procedures have […]


No Comments